An alternative to radical cystectomy for eligible patients
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Over the past several decades, organ preservation relying on combined modality treatment has become the standard of care for a variety of cancers. Trimodality therapy (TMT) relies on varied combinations of surgery, chemotherapy and radiation therapy and has proven advantageous in preserving organ function and quality of life without compromising oncologic outcomes.
A large body of evidence supports TMT across the spectrum of oncologic diseases, including breast, head and neck, lung, colorectal, gynecological and urothelial cancers.
While radical cystectomy remains the standard curative treatment for muscle-invasive bladder cancer, TMT is an underutilized, safe and effective alternative with comparable outcomes to cystectomy for patients who meet certain criteria.
Should a patient present with localized, nonmetastatic, muscle-invasive disease, the following factors are associated with favorable outcomes with TMT:
Treatment with TMT for bladder cancer involves maximal transurethral resection of bladder tumors (TURBT), followed by radiation with concurrent radiosensitizing chemotherapy. In the U.S., chemotherapy usually involves weekly cisplatin. An alternative regimen often used in Europe is mitomycin C and 5-fluorouracil, which may offer reduced impact on kidney function.
Advertisement
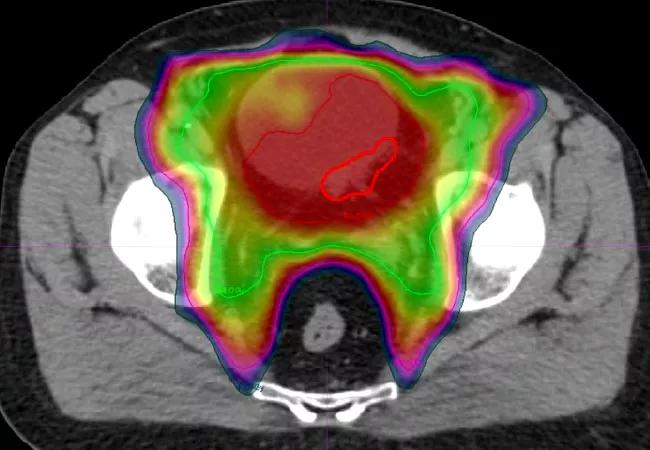
In the TMT approach, radiation oncologists typically deliver 40-45 Gy to the entire bladder, prostatic or proximal urethra and the adjacent lymph node basin in the pelvis, followed by a restaging cystoscopy with repeat TURBT and biopsies.
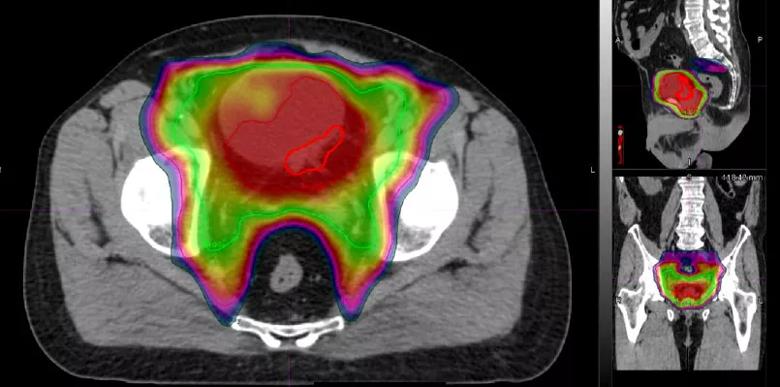
Planning CT scan for concurrent chemoradiation therapy following maximal TURBT in a bladder cancer patient; radiation dose graded by color. The red outline encircles tumor location.
If a patient demonstrates complete response, concurrent chemoradiation continues to a total dose of 64-65 Gy. A minority of patients either fail to respond or progress during chemoradiation. In such patients who display aggressive resistant histology, immediate salvage radical cystectomy is recommended.
The NCI-funded Radiation Therapy Oncology Group (RTOG) has conducted six large multi-institution trials evaluating TMT with variations of radiation dose and chemotherapy. Highlights from these studies include:
Quality-of-life and urodynamic studies show 75 percent of patients with normally functioning bladders after TMT, while long-term survivors continue to report favorable qualities of life.
Advertisement
The stepwise approach of TMT—involving TURBT, chemotherapy and radiation, coupled with post-treatment surveillance and response-adapted salvage therapy—offers patients a well-established option to retain their native bladder without compromising quality of life or treatment efficacy.
TMT should therefore be discussed as an alternative to radical cystectomy in all eligible patients, ideally at a multidisciplinary urologic oncology center.
Dr. Mian is on staff in the Department of Radiation Oncology in the Taussig Cancer Institute and Glickman Urological & Kidney Institute.
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients