Immune therapy and targeted therapies have led to durable responses and potential cures
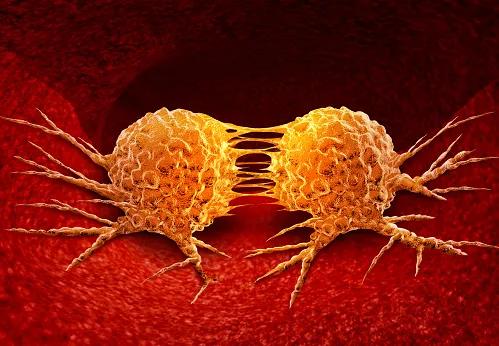
After decades of limited options for managing metastatic melanoma, advances are now occurring at a fast pace.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“It’s an exciting time to be a melanoma doctor because there are so many new treatments that have developed over the past 10 years,” says Lucy Boyce Kennedy, MD, a medical oncologist in the Taussig Cancer Institute at Cleveland Clinic. “Before 2010, no randomized controlled trial had ever shown that any drug prolonged survival in people with metastatic melanoma. Fortunately, things have changed.”
The treatment landscape shifted with the development of immune checkpoint inhibitors (ICIs) and targeted therapies.
“It’s a good time to take a step back and evaluate where we are now and where the field is going,” says Dr. Kennedy, whose commentary on improving outcomes for patients with metastatic melanoma was recently published in JCO® Oncology Practice.
Immune checkpoint inhibitors that target cytotoxic T lymphocyte antigen-4 and programmed death receptor-1 (PD-1) have ushered in a new era for cancer immunotherapy, explains Dr. Kennedy. One promising use of ICIs is the treatment regimen of ipilimumab plus nivolumab.
“The combination has been shown to lead to durable responses – including remission – even in people with stage 4 melanoma,” says Dr. Kennedy. A median overall survival of 72 months was reported in 2021 in patients who received ipilimumab plus nivolumab for metastatic melanoma.
New options continue to hit the market. In March 2022, the FDA approved a combination of the antibody relatlimab and nivolumab for metastatic melanoma. In addition to a burgeoning market for ICIs, examination of molecular drivers of melanoma has led to the development of targeted therapies, including BRAF/MEK inhibitors.
Advertisement
“Those classes of drugs — which include encorafenib plus binimetinib, dabrafenib plus trametinib, and vemurafenib plus cobimetinib — have completely transformed the way we manage patients whose melanoma has a BRAF V600 mutation,” explains Dr. Kennedy.
With so many systemic therapies available, medical oncologists may grapple with decision-making when it comes to selecting the optimal frontline therapy. Dr. Kennedy points to 2021 results of the DREAMseq Trial for guidance. The DREAMseq study compared the efficacy and toxicity of the treatment sequence of nivolumab/ipilimumab followed by dabrafenib/trametinib to the converse sequence for patients with BRAF V600-mutated melanoma.
“The study showed that patients who are treated with immune therapy first have improved overall survival compared to people who start with targeted therapy and then progress to immune therapy later,” says Dr. Kennedy.
While new therapies offer hope, areas of unmet need remain as researchers seek to refine treatment options and optimize patient selection. Dr. Kennedy notes four such areas:
Advertisement
The fast pace of advancements also creates challenges for medical oncologists who care for patients with various cancer diagnoses.
“Oncology is changing so quickly; all of the various fields are moving in parallel or different directions,” says Dr. Kennedy. “The National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology are updated as new trial data appears, but it is very difficult to keep abreast of breaking developments when things change so quickly.”
She encourages oncologists to seek advice from Cleveland Clinic and clinical research institutions that are investigating novel immune therapies and offer alternative approaches for patients in whom other treatments have been exhausted.
“Outcomes for patients with metastatic melanoma are much better than they were 10 or 15 years ago, and it’s immensely exciting to see these new developments on the horizon with the potential to cure,” says Dr. Kennedy.
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients