New baseline GFR helps predict survival rates
When patients undergo surgery for kidney cancer, they may develop new onset chronic kidney disease (CKD), i.e., CKD primarily due to surgical removal of nephrons (CKD-S). Research has shown that such patients have better survival rates than patients who have pre-existing CKD due to medical comorbidities such as diabetes (CKD-M).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Patients with medical CKD who require kidney cancer surgery tend to have progressive decline in kidney function and increased mortality rates,” says Steven Campbell, MD, PhD, Section of Urologic Oncology, Glickman Urologic & Kidney Institute. “Their comorbidities have already impacted their kidney function and since most such comorbidities are long-lasting, they continue to reduce the patient’s renal function as the years pass by.” This decline in function can be exacerbated by the surgery.
“In contrast, patients with CKD-S only have CKD because of the renal cancer surgery, and since typically they will not require further renal surgery, their kidney function can stabilize,” he continues. “They generally have good survival, similar to patients who do not have CKD at all.”
Despite evidence that patients with CKD-S tend to do well longitudinally, Dr. Campbell and colleagues noticed that past studies suggested heterogeneity among those patients, in terms of mortality rates after surgery.
In particular, some studies showed that a glomerular filtration rate (GFR) threshold value of < 45 ml/min/1.73m2 might be more discriminatory than what is typically focused on as the optimal level, namely GFR < 60 ml/min/1.73m2. With this in mind, Dr. Campbell and colleagues hypothesized that patients with CKD-S and new baseline less than GFR < 45 ml/min/1.73m2 may experience reduced survival. Their investigation was published in BJU International and they presented their data at the American Urological Association 2018 annual meeting.
Advertisement
Of the 4,246 patients in the study, 1,113 had CKD due to medical etiologies (CKD-M), 931 had CKD-S and 2,202 had no CKD even after surgery. The CKD-M patients were older than the other cohorts and had higher incidence of medical comorbidities such as hypertension and diabetes.
Dr. Campbell’s group found that non renal cancer-related 10-year survival was lowest in the CKD-M group (67 percent), and substantially improved in the CKD-S (85 percent) and no CKD groups (90 percent). Such differences held up on multivariable analysis.
Of the 931 CKD-S patients, 641 had new baseline GFRs of 45-60 mL/min/1.73 m2 and 290 had GFRs of <45 mL/min/ 1.73 m2. Those with the higher GFRs also had higher nonrenal cancer-related survival rates, 87 percent, compared to 77 percent for the low-er GFR group.
“Based on this data, we’re able say that patients with CKD-S generally have a good prognosis,” Dr. Campbell says, “but a subgroup, in which the final GFR is less than 45, faces increased mortality rates.”
Some physicians advocate for PN in all patients with localized kidney cancer whenever feasible to optimize functional outcomes. But, Dr. Campbell says in some settings this can be associated with substantial oncological and perioperative risks.
His group’s new study suggests that surgeons should instead try to estimate what postsurgery baseline GFR rates will be for renal cancer patients who do not have preexisting CKD. This may influence decisions about PN versus RN. For instance, per-forming an RN may be warranted if several criteria are met including increased oncolog-ic risk and a normal contralateral kidney that will likely provide a new baseline GFR of >45 mL/min/1.73m2.
Advertisement
“If you’re operating on a patient for renal cancer and there’s evidence they will end up with CKD-S,” says Dr. Campbell. “Most such patients will fare well after surgery, how-ever, if you think that their new baseline GFR will drop below 45, there’s reason for concern. In those cases, surgeons need to prioritize nephron-sparing approaches such as partial nephrectomy to provide the best chance for long-term survival.”
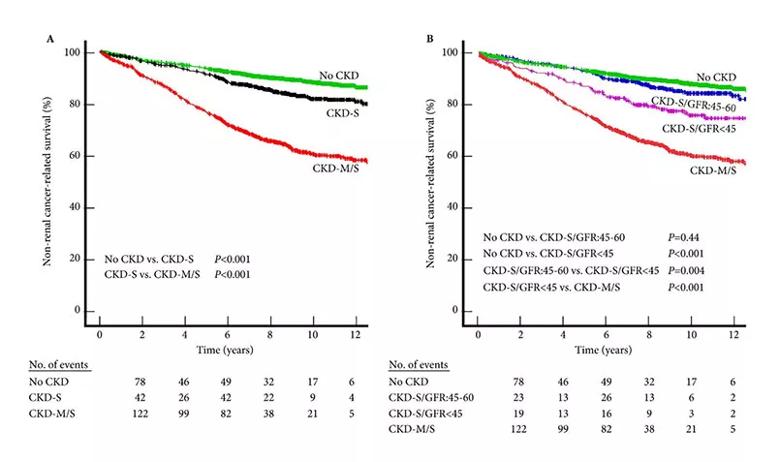
Figure 1
NRCRS after RCS based on preoperative and postoperative functional status. (A) No CKD (2 202 patients) represents patients with preoperative and new baseline GFR both of >60 mL/min/1.73 m2. CKD‐M/S (1 113 patients) represents patients with preoperative and new baseline GFR both of <60 mL/min/1.73 m2. CKD‐S (931 patients) represents patients with pre-operative GFR of >60 mL/min/1.73 m2 but new baseline GFR after surgery of <60 mL/min/1.73 m2. (B) CKD‐S is further divided into cohorts with new baseline GFR of 45–60 mL/min/1.73 m2 (641 patients) or <45 mL/min/1.73 m2 (290 patients). Non‐renal cancer‐related deaths in each 2 year interval are shown below the chart.
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients