Large consortium database from 10 academic institutions explored
Initiation of early salvage radiation therapy (SRT) following radical prostatectomy (RP) has been previously shown to reduce biochemical recurrence and distant metastases. In this new study, a large consortium database from 10 academic institutions was used to identify factors predictive of prostate cancer-specific mortality (PCSM) and all-cause mortality (ACM).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study, an update of the consortium’s nomogram published in 2007, was presented in a poster session at the American Society of Clinical Oncology’s 2017 Genitourinary Cancers Symposium by Shree Agrawal, BS, clinical research fellow at Cleveland Clinic and Case Western Reserve University medical student.
Study subjects included 2,454 patients with node-negative prostate cancer and detectable post-prostatectomy PSA (≥0.01 ng/mL) treated with SRT ± neoadjuvant/concurrent androgen deprivation therapy (N/C ADT). Cumulative incidence and Kaplan-Meier methods were used to estimate rates of PCSM and ACM, respectively. Univariate and multivariable analyses were performed by competing risks regression and Cox proportional hazards methods for PCSM and ACM.
Median follow-up was five years from SRT completion and eight years from date of RP; 24 percent had pathologic Gleason score (GS) of ≤6, 56 percent GS 7, and 19 percent GS ≥8. Fifty-six percent had extraprostatic extension (EPE), 18 percent seminal vesicle invasion (SVI), 58 percent positive surgical margins, and 16 percent received N/C ADT. Median age at RP and SRT were 62 years (IQR 56-66) and 64 years (59-69), respectively. Median SRT dose was 66 Gy (IQR 65-68) and median pre-SRT PSA was 0.5 ng/mL (IQR 0.3-1.1).
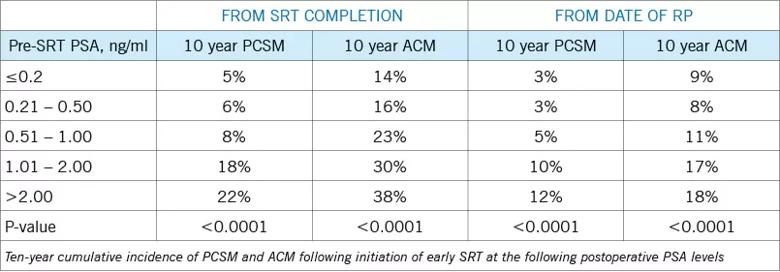
Multivariable analyses performed from SRT completion date demonstrated higher pre-SRT PSA (HR = 2.1), higher GS (GS 7 vs. ≤6: HR 2.0; GS ≥8 vs. 6: HR 3.3), and SVI (HR 2.5), respectively, were significantly associated with higher PCSM. These same variables were all significantly associated with higher PCSM and ACM rates calculated from both SRT completion date and date of RP.
Advertisement
Initiation of early SRT at lower postoperative PSA levels following RP is associated with reduced risk of PCSM and ACM, even when calculated from RP date to account for any potential lead time bias. Other factors significantly associated with PCSM include higher GS and SVI.
“Early SRT at the earliest sign of detectable PSA recurrence post-prostatectomy has a greater likelihood of improving mortality outcomes, according to our study,” Agrawal notes. “In the shared decision making between physicians and patient, additional characteristics such as Gleason score and seminal vesicle invasion are the most important factors for prostate cancer specific mortality when considering salvage radiation therapy at low postoperative PSA levels. Our hope is to soon provide clinicians a published assessment tool specific to disease characteristics when evaluating the risks and benefits of early salvage radiation therapy with respect to prostate cancer specific survival.”
“The likely indications for early SRT, as demonstrated in this study, may aid clinicians and patients in making prostate cancer care decisions, especially in the early postoperative period and when a patient elects primary treatment with radical prostatectomy,” says co-author and Cleveland Clinic radiation oncologist Rahul D. Tendulkar, MD.
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients