Treatment currently varies substantially
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy

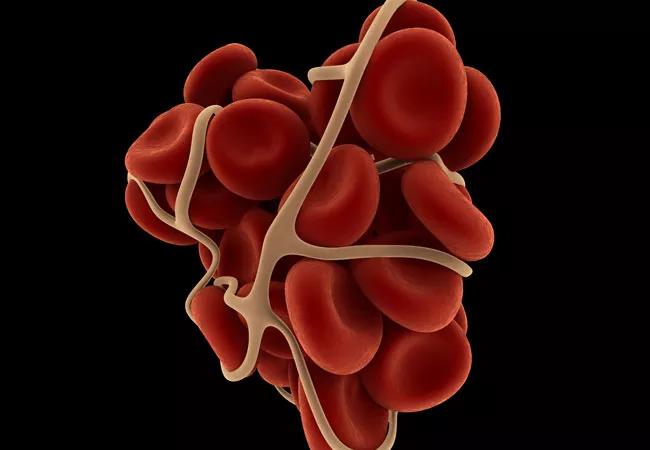
Cancer-associated thrombosis is very prevalent in patients with cancer, with some estimates suggesting that one-fifth of all patients are affected.
Multiple randomized trials have addressed best options for treatment, with a general consensus that treatment with low-molecular-weight heparins (LMWHs) is most efficacious. Therefore, current guidelines recommend anticoagulation with LMWH monotherapy for as long as six months, and possibly indefinitely, for patients with active cancer.
However, there are issues with these agents, particularly that they require injection and may be more expensive than newer anticoagulants, and that patient preference issues may lead to noncompliance.
Advertisement
In research presented at the most recent American Society of Hematology (ASH) annual meeting, my colleagues and I analyzed medical and pharmacy claims from the Humana Database to identify national patterns and variation in cancer-associated thrombosis care between Jan.1, 2013, and Dec. 31, 2014. Based on the first anticoagulant agent received, patients were classified in one of the following cohorts: LMWH, LMWH/warfarin, warfarin, or rivaroxaban. Use of other anticoagulants, including fondaparinux, heparin, apixaban and dabigatran, was low and therefore could not be appropriately evaluated.
Among 2,941 newly diagnosed cancer patients who developed venous thromboembolism (VTE) and received anticoagulation, agents used included LMWH (N = 735; 25 percent), LMWH/warfarin (N = 550; 18.7 percent), warfarin (N = 853; 29 percent) and rivaroxaban (N = 709; 24.1 percent).
This suggests a substantial variation in care, with only a quarter of patients receiving guideline-recommend therapy.
In addition, there was variation in anticoagulant therapy persistence. The median treatment durations for LMWH, LMWH/warfarin, warfarin, and rivaroxaban users were 3.29 months, 7.76 months, 8.12 months and 7.92 months, respectively. LMWH/warfarin, warfarin, and rivaroxaban users were significantly more likely to remain on their initial therapy compared with LMWH patients, with hazard ratios (HRs; 95 percent confidence interval) of 0.38 (0.32-0.45), 0.40 (0.34-0.46) and 0.42 (0.36-0.50), respectively (all p values < 0.0001).
Advertisement
Thus, this real-world analysis shows that despite guideline recommendations, warfarin and rivaroxaban are utilized nearly as often as LMWH for the treatment of cancer-associated thrombosis and that patients are less likely to persist on LMWH therapy. It is unclear whether these findings are related to patient preference, cost of medication or provider preference.
Can this variation in the care of cancer-associated VTE be reduced? In another abstract presented at ASH, we provided results from Cleveland Clinic’s experience. In 2014 we instituted a centralized service for care of cancer patients with suspected deep venous thrombosis (DVT) and/or pulmonary embolism (PE) at Cleveland Clinic Cancer Center. We hypothesized that a cancer-associated thrombosis (CAT) clinical service that provides standardized management would reduce variation in care and lower rates of recurrence, bleeding and hospitalization in this patient population.
The study population comprised 221 patients with suspected VTE seen by the CAT clinical service between August 2014 and July 2015. VTE was diagnosed in 51 patients (23 percent). Hospitalization for VTE was necessary in only 24 percent (N = 13 of 51) of cases. The mean and median costs of hospitalization for VTE (all costs) were $7,656 and $2,842, respectively, whereas the mean and median costs of outpatient VTE treatment were $1,160 and $824, respectively.
The initial treatment for 94 percent (N = 48 of 51) of patients was enoxaparin. Other treatments included warfarin (2 percent, N = 1 of 51), heparin (2 percent, N = 1 of 51) and apixaban (2 percent, N = 1 of 51). Of patients started on enoxaparin, 71 percent (N = 34 of 48) remained on it for the duration of their care. Common causes for transitioning to warfarin were financial considerations (50 percent, N = 4 of 8), patient preference (38 percent, N = 3 of 8) and poor renal function (13 percent, N = 1 of 8).
Advertisement
VTE recurred in 14 percent (N = 7 of 51) of patients with a median follow-up of 3.5 months. Recurrences occurred in 9 percent (N = 3 of 34) of patients on enoxaparin monotherapy, in 22 percent (N = 2 of 9) of patients started on or bridged to warfarin and 33 percent (N = 2 of 6) of patients taken off anticoagulation. A total of 10 recurrent VTE events occurred in seven patients. Of these, four required hospitalization. The mean and median costs of hospitalization for recurrence (all costs) were $19,528 and $18,627, respectively. The mean and median costs of initial outpatient care (excluding drug costs) for recurrent VTE were $998 and $728, respectively.
Thus, our experience suggests that centralizing care of CAT reduces treatment variation and appears to improve patient-related outcomes, including the need for VTE-related hospitalizations and recurrent VTE. Substantial cost savings can be achieved by avoiding unnecessary hospitalization for appropriate patients and by reducing recurrence and bleeding rates with appropriate therapy.
As greater knowledge regarding risk of recurrent VTE emerges, it may be possible to develop risk-adapted approaches in which higher-risk patients are treated with LMWH and lower-risk patients with oral anticoagulants, thereby improving patients’ experience and reducing the risk of recurrence and hospitalization.
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients