Injections and surgical procedures are among the therapies for patients with early and late vocal cord paralysis
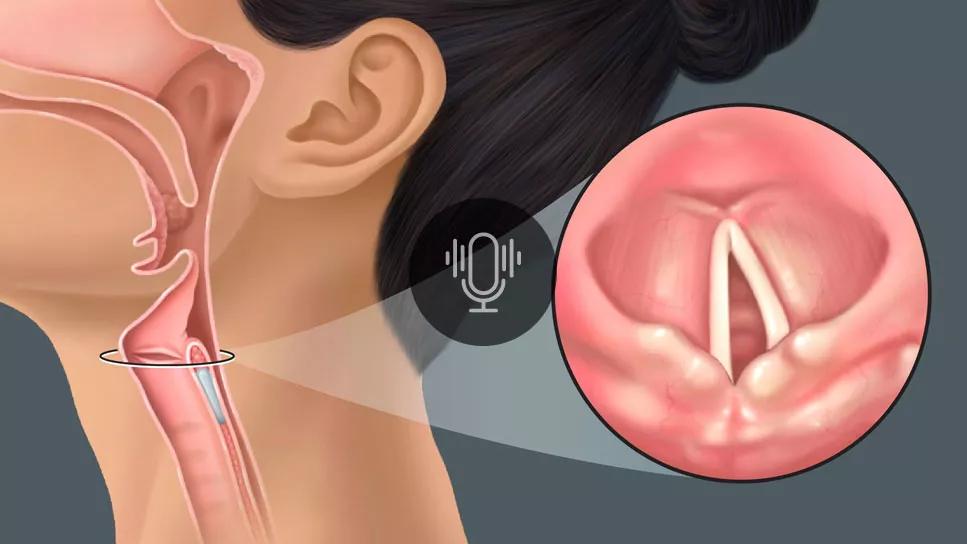
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/42a4c6f3-8f26-4e34-9530-e586ba832d1c/23-HNI-4397548-VocalCordParalysisTreatment-podcst_967x544_jpg)
vocal cord paralysis
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2241209/13504210)
Vocal cord paralysis occurs when the nerve impulses to the larynx are interrupted, causing the vocal folds to become immobilized. There’s a high likelihood of recovery if the condition is diagnosed early and the recurrent laryngeal nerve is intact. The key is to refer patients to experts who can recommend the best treatment.
“If there’s a voice problem that isn’t easily fixed or identified in the clinic, have a low threshold to send [the patient] to a voice healthcare professional – a laryngologist, a speech and language pathologist who’s been trained in voice,” says William Tierney, MD, a laryngologist and head and neck surgeon at Cleveland Clinic. “It’s a relatively small community nationally, so there’s probably someone near where you practice that has access to videostroboscopy and can identify what’s going on and then get them to the people who do the specific procedures they need.”
In a recent episode of Cleveland Clinic’s Head and Neck Innovationspodcast, Dr. Tierney provides an update on vocal cord paralysis. He discusses:
Click the podcast player above to listen to the episode now, or read on for a short edited excerpt. Check out more Head and Neck Innovations episodes at clevelandclinic.org/podcasts/head-and-neck-innovations or wherever you get your podcasts.
Advertisement
Podcast host Paul Bryson, MD, MBA: Do you want to elaborate on some of the causes of vocal cord paralysis and some of the predicaments that patients may undergo that then lead them to us?
Dr. Tierney: The iatrogenic causes of vocal cord paralysis, or vocal fold paralysis, are neck surgery, thoracic surgery and then anything that could potentially stretch the recurrent laryngeal nerve, which if you’ll remember from anatomy has sort of a tortuous path going down into the thorax on the left, looping under the ligament arteriosum and then coming back up to the larynx. And so anywhere along that line, you can have interruption or irritation of the nerve.
And so, the surgical procedures we think of are certainly any esophageal procedures, as the nerve runs in the tracheoesophageal groove on its way back up to the larynx. Thyroid surgery is one of the more common things that we have to think about in our world. Nodal laryngology, head and neck surgery. But then really any thoracic procedure has the potential to stretch the nerve.
We also see a certain amount of vocal fold paralysis or hypo-mobility, where we’re not sure necessarily that it’s paralyzed versus immobile, after some other common procedures like intubation. The thought being that the nerve can be put under some pressure by an endotracheal tube within the larynx and you can have a temporary or permanent immobility following an intubation, either short term or long term.
There are some other causes, but I think those are sort of the common ones that everybody should be aware of and look out for.
Advertisement
Advertisement
With a wide scope of skills, comprehensive otolaryngologists care for patients of all ages in the community
Research on children with UHL explores the quality-of-life benefits and outcomes of cochlear implants
A look at how custom-fitted oral appliances work and when they’re a good fit for patients
Subtle information gleaned from clinical examinations prompted concern
A new single-port system well-suited for oropharyngeal cancer treatment
Challenging case requires outside-the-box approach
Collaborative and multidisciplinary approach necessary for treatment
The tri-vector gracilis procedure uses a thin muscle from the thigh to help create a natural mimetic smile