Simple protocol changes can shorten waits for care

Simple, inexpensive changes in how emergency departments handle cancer patients who present with fever can significantly shorten those patients’ wait for antibiotic administration and decrease their hospital stay, a Cleveland Clinic study has found.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The changes involve elevating caregivers’ awareness of the urgent nature of febrile neutropenia (FN), and standardizing and accelerating the triage and treatment process.
“It took less than half a year to institute these changes, and their benefits have persisted for years afterward,” says Mikkael Sekeres, MD, MS, Director of Cleveland Clinic’s Leukemia Program.
The research results were published in November 2015 in the Journal of Oncology Practice.
FN — defined as an absolute neutrophil count > 0.5 x 109/L and body temperature ≥ 38.3°C, or temperature > 38.0°C for longer than one hour — is a frequent and serious complication of chemotherapy. Mortality rates in excess of 55 percent have been documented in FN patients with multiple comorbidities.
“It’s a life-threatening emergency similar to heart attack or stroke,” Dr. Sekeres says.
Findings from randomized clinical trials support early use of broad-spectrum antibacterial drugs to decrease mortality and morbidity in FN patients. Guidelines from the American Society of Clinical Oncology and the Surviving Sepsis Campaign recommend administering the initial antibiotic dose within one hour after triage.
However, there is little data about the quality and value of prompt antibiotic delivery to FN patients in the emergency department (ED), and best care practices for these patients are undefined. Awareness of FN’s urgent nature and the immediate need for antibiotic administration is variable among healthcare workers who treat cancer patients.
Advertisement
Since chemotherapy regimens are increasingly delivered in outpatient settings, FN patients are more likely to seek treatment in the ED, where they may encounter treatment delays due to crowding, competition with patients assessed as higheracuity, and/or inconsistent definitions of and treatment protocols for FN.
Dr. Sekeres and his Cleveland Clinic collaborators hypothesized that creating a formal FN pathway would reduce the time to antibiotic administration and produce other benefits.
Their prospective review of medical records of adult cancer patients who presented to Cleveland Clinic’s ED with fever identified significant delays in three areas: time from ED registration to physician evaluation, availability of neutropenia testing results and time to antibiotic administration.
In response, the researchers designed and implemented a protocol that:
• Reclassified FN on the Emergency Severity index as the equivalent acuity of a cerebrovascular accident or myocardial infarction
• Triaged FN patients to private rooms at ED registration rather than a communal waiting room
• Standardized the definition of FN at all inpatient and outpatient cancer center and hospital sites
• Provided cancer patients with a wallet-sized FN alert card with specific febrile instructions, to prompt ED personnel to initiate the FN protocol
• Created an FN “chief complaint” category and a standardized order set in the hospital electronic medical record system to eliminate treatment variability
• Directed that FN antibiotics be administered prior to complete blood count confirmation of neutropenia, and that they be made available in ED Pyxis® machines to avoid delays in transport from the central pharmacy
• Educated ED and cancer center personnel about the FN regimen via in-service training and staff meeting updates
Advertisement
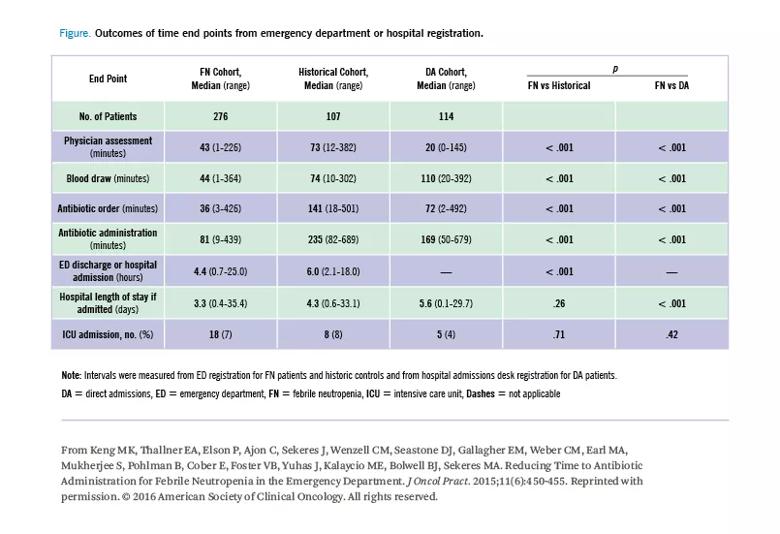
After implementation of the FN protocol, the researchers compared outcomes of all adult cancer patients who presented to Cleveland Clinic’s ED with fever between June 2012 and June 2013 with a historical cohort of similar febrile cancer patients admitted to the ED pre-protocol, and with a group of febrile cancer patients admitted directly to the hospital’s inpatient oncology service.
The study’s primary outcome measure was the time to antibiotic administration (TTA), with a target of 90 minutes. (The ASCO and Surviving Sepsis 60-minute TTA recommendations had not been issued when the Cleveland Clinic study began.) Secondary outcomes were the intervals from ED registration to physician exam, antibiotic order placement, and ED discharge or hospital admission; hospital length of stay; and whether the patient was admitted to the intensive care unit.
In the historical FN patient cohort, median TTA was 235 minutes, and in the direct admission cohort it was 169 minutes. Institution of the FN awareness and expediency protocol decreased median TTA to 81 minutes, a reduction of two-thirds compared with the historical cohort and one-half compared with the direct admission group (p < .001 for both).
The FN protocol was associated with significantly shorter median antibiotic order placement times (36 minutes, compared with 141 minutes for the historical cohort and 72 minutes for the direct admission group), and median hospital lengths of stay (3.3 days, compared with 4.3 days for the historical cohort and 5.6 days for direct-admission patients; p < .001 for all).
Advertisement
Follow-up research 18 months after initiation of the FN protocol showed that median times to all study end points had continued to decline, with time to antibiotic order down to 22 minutes and TTA reduced to 68 minutes.
“For the first time, we were able to demonstrate that instituting a number of simple interventions decreased the time it took for febrile neutropenia patients to receive antibiotics from four hours to a little over an hour,” Dr. Sekeres says. “With the FN pathway, we were able to decrease length of hospitalization by approximately one day. These changes produced real, lasting value for our patients. They are relatively easy to enact, and could translate to an improved patient experience and reduced healthcare costs.”
Photo Credit: ©Russell Lee
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients