For the first time, outcomes linked to scoring system
When patients receive neoadjuvant chemoradiation (CRT) followed by proctectomy for locally advanced rectal cancer, variability in treatment response ranges from complete histologic regression to progression of disease. Most patients have a partial response, the implications of which are unclear.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As a step toward standardizing reporting and treatment response information, the American Joint Committee on Cancer (AJCC) and the College of American Pathologists (CAP) published guidelines in 2010 for grading rectal cancer response to neoadjuvant CRT. The four-grade scoring system was designed to include two partial response grades, with the premise that incremental improvement in response serves as a surrogate for better outcomes.
While these guidelines were established based on expert consensus, the clinical relevance of the grading system as related to oncologic outcomes had not been validated and remained unknown until recently.
A retrospective cohort study of more than 500 patients conducted at Cleveland Clinic and published in Diseases of the Colon & Rectum is the first study to delineate the AJCC/CAP regression grade as an independent prognostic factor. Primary outcome measures were overall disease-free survival, cancer-specific mortality and cumulative recurrence rate.
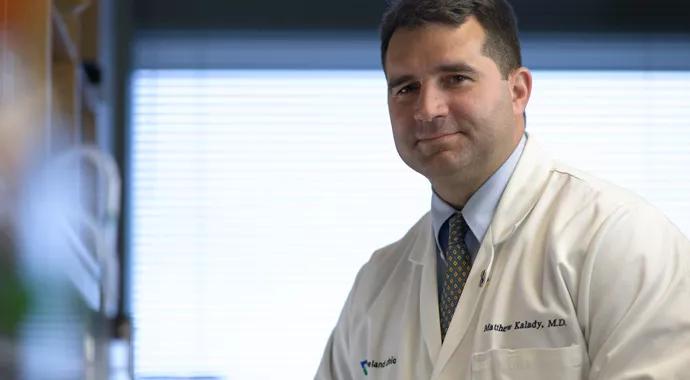
“We looked at the AJCC/CAP grading, which ranges from 0 to 3, in relation to survival and determined that each of the categories has a sequential survival advantage,” says Matthew Kalady, MD, a surgeon in Cleveland Clinic’s Department of Colorectal Surgery and the paper’s senior author. “This validation allows us to talk to patients about what their prognosis is in a more concrete way and could influence wider adoption of the AJCC/CAP scoring system.”
As Dr. Kalady and colleagues state in their study: “These findings highlight the importance of reporting tumor regression according to these criteria so that this important prognostic information is widely available to clinicians who treat rectal cancer.”
Advertisement
The retrospective cohort study was based on data from Cleveland Clinic’s prospectively maintained colorectal cancer database of patients with primary rectal adenocarcinoma who underwent neoadjuvant therapy between 1992 and 2012. Researchers defined the cohorts based on the AJCC/CAP tumor regression grading system.
Of the 538 patients included in the study, the AJCC/CAP grading was:
The researchers determined using Kaplan-Meier analysis that AJCC/CAP grade was associated with significant differences in overall survival, disease-free survival, and cumulative recurrence (p < 0.001 for all).
Five-year overall survival rates (p < 0.001) were:
Five-year disease-free survival rates (p < 0.001) were:
Five-year overall recurrence rates (p < 0.001) were:
After using Cox regression analyses to adjust for significant covariates, including pathologic stage, AJCC/CAP grading remained an independent predictor of overall survival, disease-free survival, and cumulative recurrence (p < 0.001 for all).
“Even though the AJCC/CAP grading system has been in existence since 2010, no one had put numbers on it to say what the outcomes were,” Dr. Kalady says. “The idea has always been the better the grade, the better the survival — but we had no data to say what that meant specifically. Now we have specific numbers that can be attached to the scoring.”
Advertisement
Dr. Kalady’s team first reported the research results at the American Society of Colon and Rectal Surgeons (ASCRS) meeting in 2014. The presentation won an award from the Canadian Society of Colon and Rectal Surgeons, and “our colleagues were excited about it and said it was something they plan to use with their patients,” Dr. Kalady says.
At Cleveland Clinic, the clinical validation of the AJCC/CAP grading system means additional evidence-based prognostic information that can be considered at multidisciplinary tumor board meetings where oncologists, surgeons, radiation oncologists and other specialists review rectal cancer cases before and after surgery.
“Patients appreciate knowing what the expectations may be, and now we have more concreate information to share with them,” Dr. Kalady says. “I also tell them every patient is a bit different, but if we treated 100 people, this is what we would expect across the board.”
Looking forward, Dr. Kalady and colleagues are continuing to analyze their patient databases to look for “subsets of nuances” within the grading system that may trigger future research efforts.
Dr. Kalady is a member of Cleveland Clinic’s departments of Colorectal Surgery, Cancer Biology, and Stem Cell Biology and Regenerative Medicine. He also is an Associate Professor of Surgery at Cleveland Clinic Lerner College of Medicine. He can be reached at kaladym@ccf.org or 216.445.2655.
Photography credit: ©Russell Lee
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients