Which results in better outcomes?

By Jihad Kaouk, MD, and Pascal Mouracade, MD, MPH, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The concept of off-clamp partial nephrectomy (PN) to avoid ischemic injury to the healthy parenchyma of operated kidneys has been described in the literature for open, laparoscopic and robot-assisted procedures.
However, true comparisons of the effectiveness of off-clamp and renal arterial clamping are difficult, especially in retrospective studies. To more accurately compare off-clamp and arterial clamping techniques, we conducted a large retrospective analysis comparing perioperative morbidity and functional outcomes during robot-assisted partial nephrectomy (RAPN) in carefully matched groups.
This research was presented at the American Urological Association 2017 annual meeting.
The study evaluated histories of 940 patients who underwent RAPN between 2007 and 2016 for cT1a tumors. Those with solitary kidney or multifocal tumors were excluded. Researchers matched 309 on-clamp cases to 103 off-clamp, comparing clinicopathological characteristics, perioperative morbidity and late functional outcomes between the groups.
All RAPN procedures were performed with the da Vinci® surgical system. The renal artery was routinely localized and dissected. Cold ischemia and selective vascular dissection were not used. All tumor excisions were performed with a thin parenchymal margin resection. After tumor resection, an inner parenchymal layer sutured reconstruction was performed, followed by capsular sutures for approximation of the renal defect and hemostasis.
Patient demographics (age, gender, race, body mass index, Charlson comorbidity index , American Society of Anesthesiologists score, baseline estimated glomerular filtration rate [e-GFR], baseline chronic kidney disease [CKD] stage) were collected. We also collected clinical tumor characteristics (R.E.N.A.L. nephrometry score, radiological maximum tumor diameter, hilar location, laterality, malignancy, American Joint Cancer Committee staging and tumor grade).
Advertisement
Primary outcomes were decline in e-GFR (calculated according to MDRD formula), e-GFR preservation and CKD upstaging. Decline in e-GFR was defined as the difference between postoperative (three to 12 months) and baseline measurements. E-GFR preservation was calculated as postoperative divided by baseline readings. CKD was defined according to the Kidney Disease Outcome Quality Initiative-Chronic Kidney Disease.
Secondary outcomes included operative time, estimated blood loss (EBL), transfusion rate, postoperative Clavien complications, surgical reoperation, 30-day readmission, surgical margin status and excisional volume loss.
Researchers found significant differences between the two groups in excisional volume loss (median, 7.08 vs. 3.51 cm3, p<0.01), e-GFR decline (median, -9.7 vs. -2.2 ml/min/1.73m2, p<0.01), percent of e-GFR preservation (median, 87 percent vs. 97 percent, p<0.01), and CKD upstaging (36.5 percent vs. 23.3 percent, p=0.01), all in favor of the off-clamp group. Excisional volume loss (p=0.01), off-clamp approach (p=0.01), and age (p=0.02) were predictors of renal function preservation, whereas excisional volume loss (OR=1.035, CI 95% [1.015-1.06], p<0.01) predicted CKD upstaging.
Secondary endpoints were comparable between the groups.
Preoperative factors including age, race, BMI, ASA and laterality did not affect the surgeon’s decision to select an on- or off-clamp approach. But tumor size, R.E.N.A.L score and Charlson comorbidity index were considered influences on the selection of approach. For example, larger tumor size in one group, which required an incrementally larger resection volume of adjacent normal kidney to ensure complete excision, may have resulted in less functional kidney preservation following surgery. Parenchymal volume loss is believed to correlate with excisional volume loss, especially in small renal tumors.
Advertisement
We believe that excisional volume loss is a surrogate measure providing insight into parenchymal volume loss, which is for the time being impractical to measure directly. We think that an off-clamp approach promotes a tendency to limit parenchymal resection in order to reduce bleeding, though less excisional volume did not affect the positive surgical margin in our series.
In this study, the off-clamp group experienced better renal function preservation compared to the on-clamp group, despite the on-clamp group having a median ischemia time of less than 20 minutes.
The clinical significance of these findings will require further investigation, but we believe that surgeons should strive to limit both ischemic time and the extent of healthy tissue excision when performing partial nephrectomy.
In cases that require clamping, ice-cooling techniques may help further preservation of kidney function.
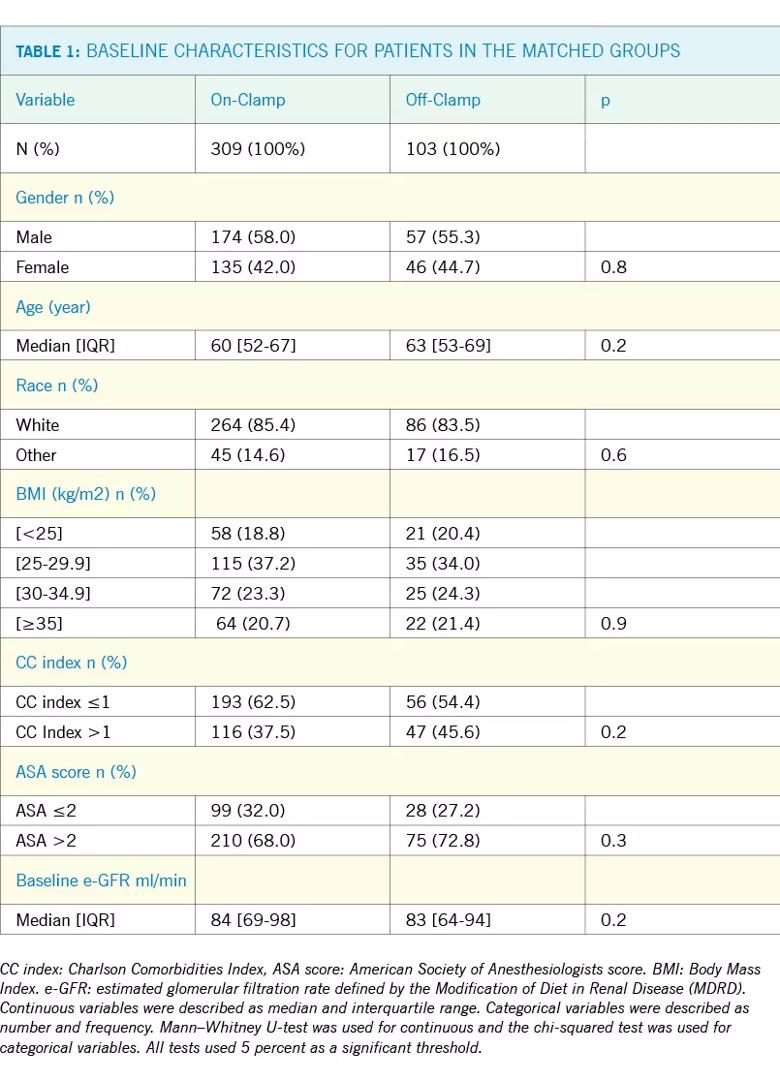
Table 1 shows baseline patient characteristics for on-clamp and off-clamp groups after matching. There were no differences in gender (p=0.80, age (p=0.2), race (p=0.6), BMI subclass (p=0.9), CCI index (p=0.2), ASA score (p=0.3) and baseline e-GFR (median 84 vs. 83 ml/min/1.73m2, p=0.2) between the two matched groups.
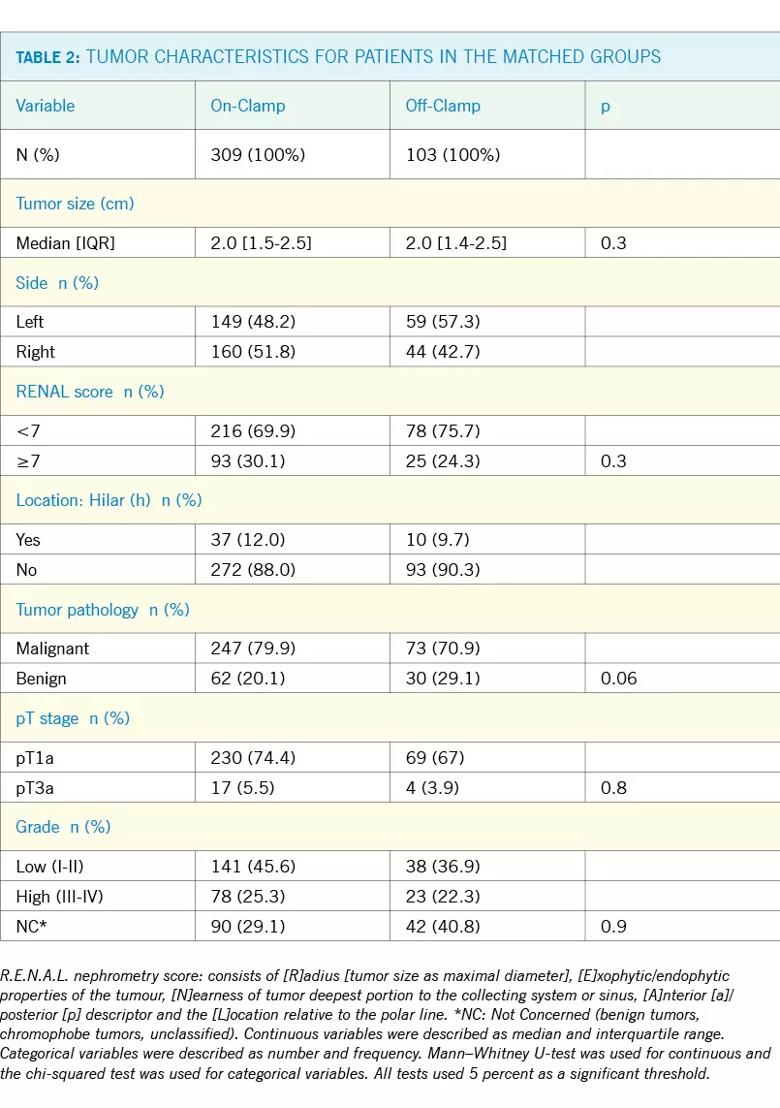
Table 2 shows the tumor characteristics for on-clamp and off-clamp groups after matching. There were no difference in tumor size (median, 2.0 vs. 2.0 cm, p=0.3), laterality (p=0.1), R.E.N.A.L score (p=0.1), hilar (h) location (p=0.5) and pT stage (p=0.8) between the 2 matched groups.
Advertisement
Dr. Kaouk is a consultant for Endocare and Intuitive. No competing financial interests exist for the other authors.
Dr. Kaouk is Director, Center of Advanced Laparoscopic and Robotic Surgery, at Glickman Urological & Kidney Institute, where Dr. Mouracade is completing a urology fellowship. Julien Dagenais, MD; Onder Kara, MD; Matthew Maurice, MD; Ryan Nelson, DO; Khaled Fareed, MD; Robert Stein, MD; and Amr Fergany, MD, also contributed to this research.
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients