Hip pain case illustrates limitations of CT guidance
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 50-year-old woman presented to an outside institution with bilateral hip pain. An MRI of the pelvis showed multiple marrow-infiltrating lesions in the pelvic bones and spine, and a diagnosis of metastatic disease was made. Staging CT studies did not reveal a primary tumor in the chest, abdomen or pelvis. The bone lesions seen on MRI were not visualized on CT of the abdomen and pelvis. A CT-guided blind biopsy of the pelvic lesions was done.
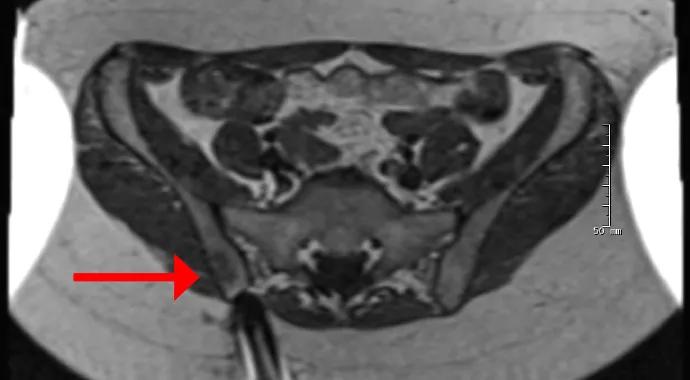
Immediately after receiving a nondiagnostic biopsy result, the patient came to Cleveland Clinic for a second opinion. We performed MRI-guided biopsy of the pelvic lesions (Figure 1), and histology showed extensive granulomatous inflammation consistent with sarcoidosis and no evidence of a neoplasm.
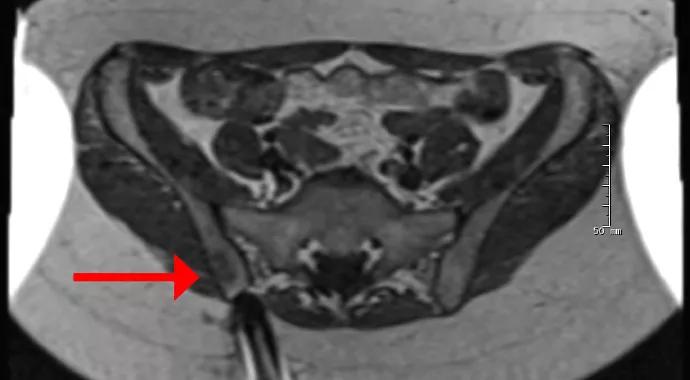
Figure 1. T2-weighted MRIs during and after the biopsy. On the left is an axial image showing the needle approaching the bone lesion (arrow). The middle image shows the needle tip within the lesion. The right image, which is from a post-biopsy coronal STIR sequence, shows the needle tracks (two bright round areas denoted by arrows) from the patient’s two biopsies, which are surrounded by abnormal signal consistent with a lesion.
Percutaneous or open surgical biopsy is often required to confirm the diagnosis of an indeterminate or aggressive bone lesion. Percutaneous needle biopsy of bone lesions is a safe and accurate method with a very low (1.1 percent) complication rate (Cancer. 2000;89:2677-2686). Real-time CT fluoroscopic guidance is typically used, often with low-dose techniques to limit radiation exposure. Nearly all primary and metastatic bone lesions are visible on CT, which allows accurate needle localization inside the lesion. In rare cases, however, lesions cannot be visualized on CT despite obvious findings on MRI. In these cases, MRI can be a safe and reliable alternative for guiding the biopsy.
Advertisement
Compared with CT, MRI has several advantages for guiding biopsies, including superior soft tissue contrast, unique three-dimensional imaging capabilities and a lack of ionizing radiation. The main disadvantages are the long scanning time and the need for MRI-compatible devices, including biopsy needles. During CT guidance of a bone biopsy, scanning time is often less than a second, whereas MRI guidance requires three to four minutes of scanning at each step, which can add up to 60 to 90 minutes or more in complicated cases.
For the occasional patient who would benefit from image-guided biopsy of a bone lesion visible only on MRI, Cleveland Clinic is one of the few medical centers in the world offering this distinctive service. MRI-guided biopsies are performed under conscious sedation in the MRI suite on our main campus.
Dr. Ilaslan is a musculoskeletal radiologist in the Department of Diagnostic Radiology and Associate Professor of Radiology at Cleveland Clinic Lerner College of Medicine.
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients