Study compares open versus laparoscopic abdominoperineal resection outcomes
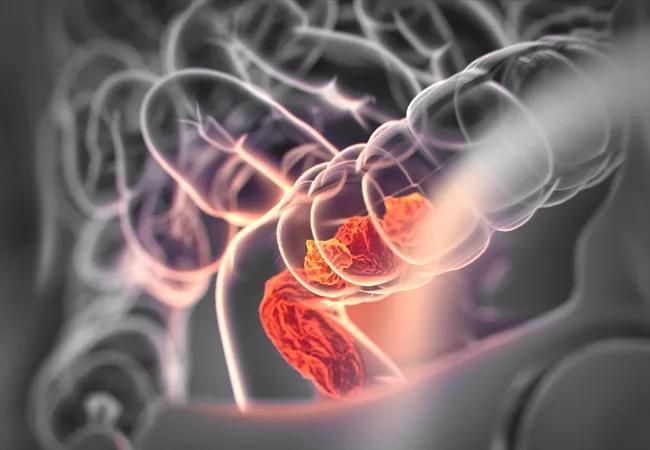
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/adbe2db1-7d1c-450b-90f4-4c45d2d85096/18-DDI-5519-Rectal-Cancer-Hero-Image-650x450pxl_jpg)
18-DDI-5519-Rectal-Cancer-Hero-Image-650x450pxl
A minimally invasive approach to abdominoperineal resection (APR) for rectal cancer produces similar long-term oncological outcomes to an open APR procedure, but with less risk for wound infections and shorter hospital stays, new data from Cleveland Clinic indicates.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We showed that the cancer-related outcomes – which is the utmost priority – were the same. But with a minimally invasive approach you get the added benefits of better short-term perioperative outcomes,” says study senior author Scott R. Steele, MD, MBA, Chair of Cleveland Clinic’s Department of Colorectal Surgery.
The findings, from 452 patients with primary rectal cancer who underwent either open or minimally invasive APR at Cleveland Clinic between 2000 and 2016, represent the largest and longest experience to date for the APR comparison.
In rectal cancer, anal sphincter-preserving operations combined with neoadjuvant chemoradiation are increasingly performed and are preferable when possible. However, APR is still the more appropriate option for at least 30% of patients with low-lying rectal cancers — those with poor sphincter function, with tumors involving the sphincters, or with tumors whose location precludes obtaining clear negative distal resection margins.
Previous studies demonstrating worse outcomes for APR compared to sphincter-preserving procedures may have been affected by selection bias since patients with more advanced tumors are more likely to be offered APRs. At the same time, studies that have shown equivalent outcomes for minimally invasive laparoscopic and open procedures for rectal surgery have combined sphincter-preserving resections with APRs.
“There’s not a lot of data comparing APR to APR by surgical approach,” Dr. Steele says. “We looked at a set of relatively uniform tumors, all undergoing APR with either minimally invasive or open approaches. Our large database allowed us to compare apples to apples.”
Advertisement
Of the total 452 patients, 372 underwent open APR operations while 80 had minimally invasive procedures — 48 laparoscopic and 32 robotic — performed by a total of 26 colorectal surgeons.
Most patient characteristics were similar between the two groups, except that those who had open procedures tended to be more overweight (body mass index 28.6kg/m2 vs. 27.02kg/m2, p = 0.036), and were less likely to receive neoadjuvant radiation (67.5% vs. 81.3%, p = 0.01).
Surgery time was significantly longer with the minimally invasive procedures: 287 minutes versus 200 minutes for open procedures (p < 0.0001). “With minimally invasive approaches, especially in your initial experience, you tend to go slower and the setup is longer,” Dr. Steele notes. “However, over the years the difference in operative time between open and minimally invasive has narrowed.”
Estimated blood loss was higher with open operations (679mL vs. 354mL, p = 0.056). Intraoperative adverse event rates for the two procedure types were similar (11.8% vs. 13.8%, p = 0.706).
Postoperatively, hospital length of stay was significantly shorter for patients who underwent the minimally invasive procedures, averaging 6.6 days compared to 9.5 days following the open procedures (p < 0.001). Rates of postoperative complications didn’t differ significantly (34.5% open versus 27.5% minimally invasive, p = 0.177).
Perineal wound infections were significantly more common following open procedures (12.5% vs. 2.5%, p = 0.008). There were 6 deaths in the open procedure group and none in the minimally invasive cohort. Readmission rates didn’t differ.
Advertisement
There were also no significant differences in mean number of harvested lymph nodes (21.7 open versus 22.2 minimally invasive, p = 0.7), mean distance to radial margin (1.48cm vs. 1.37cm, p = 0.4), or distance to distal margin (4.8cm vs 4.1cm, p = 0.09).
Average tumor size was significantly larger in the open procedure group (3.8cm vs 3.3cm, p = 0.05). There were no significant differences in the rates of involved radial margins (10.8% vs 6.3%, p = 0.376) or in rates of involved distal margins (0.5% vs 0%, p = 1).
At a median follow-up of 74 months, disease recurrence rates were 19.4% for open versus only 7.5% for minimally invasive (p = 0.001). Disease-free survival rates at 5 years and 10 years were 77.6% and 56.5%, respectively, for minimally invasive versus 63.2% and 47.4% open (p = 0.091). Overall survival rates at 5 and 10 years were 80% and 65% for minimally invasive and 70% and 52%, respectively, for open (p = 0.344).
No major differences were seen between laparoscopic and robotic minimally invasive approaches.
Still, Dr. Steele points out that there are some situations in which open APR procedures are more appropriate, such as with a large bulky tumor for which adequate margins can’t be obtained through a minimally invasive approach; difficulty with visualization; or if there are safety concerns regarding use of a minimally invasive procedure that the open approach would ameliorate.
Ultimately, Dr. Steele says, “the areas you resect and the principles that you follow should be the same whether you do a minimally invasive or an open approach. The overriding principle for anything to do with cancer is to make sure that patients get the best possible cancer-related outcomes.”
Advertisement
Advertisement
First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses
Global R&D efforts expanding first-line and relapse therapy options for patients
Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels
A case study on the value of access to novel therapies through clinical trials
Findings highlight an association between obesity and an increased incidence of moderate-severe disease
Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456
Key learnings from DESTINY trials
Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients