A robotic approach may be the right choice for the toughest cases
By Daniel Ramirez, MD; Benjamin Cohen, MD; Venkatesh Krishnamurthi, MD; and Georges-Pascal Haber, MD, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Treating renal neoplasm with associated inferior vena cava (IVC) thrombus presents a challenging surgical endeavor. Manifestation of tumor thrombus within the renal vein or IVC occurs in 4 to 10 percent of patients with renal cell carcinoma (RCC), and traditionally these patients have been managed with open surgery due to the complex nature of the procedure.
Several staging systems exist to describe the extent of the IVC thrombus. Various series have described the management of patients with level I-II tumor thrombi via a laparoscopic approach. With surgeons’ growing experience using robotic techniques, renal tumors with associated tumor thrombi are increasingly managed with a robot-assisted approach at high-volume centers of excellence. Nonetheless, there is a paucity of literature describing robotic techniques for treatment of level III tumor thrombi.
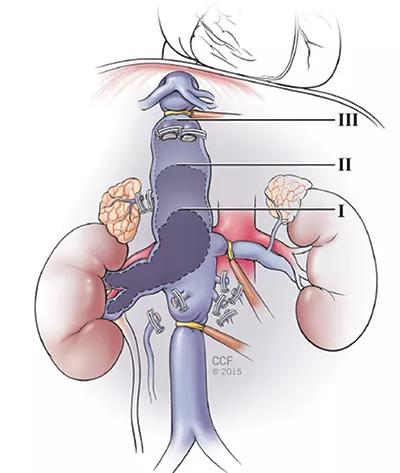
Figure 1. Intracorporeal control of IVC with Rommel-style tourniquets.
The primary steps for right-sided radical nephrectomy and level III IVC thrombectomy include early ligation of the right renal artery in the intra-aortocaval space, circumferential control of the IVC above and below the tumor thrombus, control of the left renal vein, and use of intraoperative transesophageal and intraperitoneal ultrasound to delineate the extent of the tumor prior to IVC cross-clamping (Figure 1).
The patient is a 75-year-old Caucasian man with a medical history significant for chronic kidney disease stage 3 and prior right hip replacement. He initially presented with abdominal pain and gross hematuria. Cross-sectional imaging for hematuria workup revealed a central 9.8-cm right-sided renal mass with an associated suprarenal IVC tumor thrombus. MRI performed two weeks prior to surgery for staging of the thrombus showed a tumor thrombus extending into the retrohepatic IVC above the level of the short hepatic veins (Figures 2 and 3) and associated with retroperitoneal lymphadenopathy.
Advertisement
| Figure 2. Axial MRI demonstrating cranial extent of the tumor thrombus. | Figure 3. Coronal MRI demonstrating cranial extension of the tumor thrombus. |
|---|---|
| Figure 2. Axial MRI demonstrating cranial extent of the tumor thrombus. |
The patient’s metastatic workup was negative. Preoperative creatinine and hemoglobin levels were 1.53 mg/dL and 11.3 g/dL, respectively. Consultation with medical oncology was obtained prior to surgery for consideration of preoperative neoadjuvant immune-modulation treatment. The consensus was to proceed with robotic radical right nephrectomy, retroperitoneal lymph node dissection and IVC tumor thrombectomy, with close observation of the pulmonary lesions.
It is generally recommended to repeat cross-sectional imaging for reassessment of the tumor thrombus within two weeks prior to surgery to determine if there has been any interval growth. In patients with level III thrombi, the central focus of the operation is meticulous dissection and control of the IVC in order to perform successful cavotomy, tumor thrombus extraction and caval reconstruction while minimizing bleeding. In our case, four short hepatic vessels required division (Figure 4). Total operative time was 353 minutes and estimated blood loss was 150 cc. No intraoperative or postoperative transfusions were required. Extended operative time was expected as this was the first robotic approach for a level III thrombus performed at our institution.
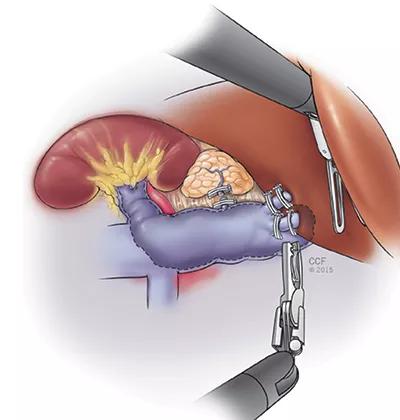
Figure 4. Control and ligation of short hepatic vessels for intrahepatic IVC control.
Postoperatively, the patient was taken to the post-anesthesia care unit for anesthesia recovery, and was subsequently admitted to the regular nursing floor. The patient was ultimately found to have pT3bN1 disease, and final histological assessment revealed nuclear grade 3 collecting duct RCC.
Advertisement
The patient advanced to clear liquids several hours after surgery and was given a regular diet on postoperative day two. He was discharged on postoperative day three. The patient’s hemoglobin reached a nadir of 9.3 g/dL immediately after surgery and was 9.5 g/dL on the day of discharge. Hemoglobin and creatinine levels at one-week follow-up were 10.6 g/dL and 1.52 mg/dL, respectively. The patient received prophylactic low-molecular-weight heparin for 28 days after surgery.
Robotic surgery for management of RCC and associated level III IVC thrombi is feasible in select patients. As with any novel technique, further experience with long-term followup is necessary. At high-volume institutions, this approach appears to be a viable option, with potential lower EBL and shorter convalescence compared with open surgery. Nevertheless, open surgery should currently remain the standard of care for patients with this complex condition, as the main goals for success remain safety and cancer control.
Dr. Cohen is chief resident in the Department of Urology.
Dr. Krishnamurthi is a staff member of the Department of Urology and of the Transplant Center.
Dr. Haber is a staff member of the Department of Urology.
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients