Registry linkage study reports on incidence, risk factors and survival
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/84c6422f-997a-4834-a65b-a119b061a92b/Valapour_LT_lung_cancer_jpg)
Valapour_LT_lung_cancer
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With the increasing use of lung transplantation for patients with end-stage lung disease comes an increase in the long-term complications of transplant, including the risk of lung cancer. My colleagues and I, including first author Matthew Triplette, MD, MPH, recently conducted a registry linkage study to explore this poorly understood increase in risk and published our results in the American Journal of Transplantation.
We used data from the Transplant Cancer Match (TCM) study, which links U.S. Scientific Registry of Transplant Recipients (SRTR) with 17 state and regional cancer registries, to quantify lung cancer risk, histology, stage, treatment and survival in lung transplant recipients compared with the general population as well as to identify risk factors for its development.
Our cohort of 8993 patients was comprised of 53 percent male recipients, and the median age at time of transplant was 54 years. Forty-five percent had undergone single lung transplantation and the remainder a double lung procedure. The top three indications for transplantation were COPD (34 percent), idiopathic pulmonary fibrosis (IPF) (25 percent) and cystic fibrosis (16 percent). Of the 77 percent of recipients with available smoking data, 64 percent had a pretransplant history of smoking.
We found that recipients of a single lung transplantation had a 13-fold increased risk of lung cancer (standardized incidence ratio [SIR] 13; 95% CI, 11-15) in the native lung compared with similar persons in the general population who did not have a transplant. Risk of lung cancer was about five times higher for all lung transplant recipients compared with the general population (SIR 4.8; 95% CI, 41.-5.5). The below table summarizes our results.
Advertisement
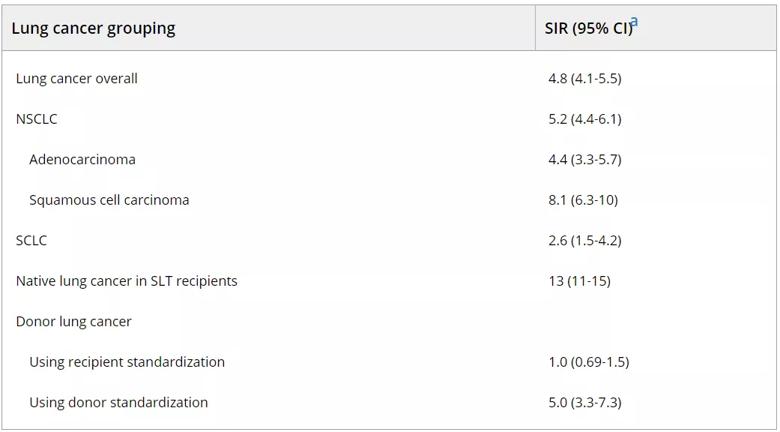
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b78d267e-2acc-432a-8a9b-fbd4e5b72bb2/valapour-table_png)
Republished with permission from the American Journal of Transplantation.
The following factors were significantly associated with increased risk for lung cancer in recipients of a single lung transplant: history of cigarette smoking pretransplant, older age at transplant, lower education level and longer time since transplant. A vast majority of native lung cancers (90 percent) occurred in recipients with COPD or IPF, but only IPF was associated with a significantly higher risk (adjusted IRR 1.6; 95% CI, 1.0-2.6).
Compared with lung cancer patients in the general population, transplant recipients with lung cancer were younger (P < 0.001), more likely to have localized disease (28 versus 20 percent, P = 0.04), and more likely to be treated with surgery (37 vs 26 percent, P = 0.05). Despite presenting at earlier stages, survival was shorter for transplant recipients than for other patients (median 153 versus 245 days, P < 0.001). All-cause and cancer-specific mortality was higher for transplant recipients.
Our findings suggest that pre-existing damage in the native lung contributes significantly to the increased risk of lung cancer in lung transplant recipients. Our results also may indicate that transplant-related factors (e.g., immunosuppression) contribute to carcinogenesis, as our analysis showed that native lung cancer risk increased with time from transplant and that risk increased for transplanted lungs as well. We also observed a difference in tumor histology, with a disproportionate increase in squamous cell cancer following transplantation, suggesting that distinct oncogenic mechanisms may be involved.
Advertisement
The increase in mortality despite the earlier stage at presentation and greater use of surgical intervention may reflect a more aggressive cancer biology with loss of immune control of cancer progression. Transplant-related comorbidities such as chronic allograft dysfunction and infection likely also contribute to the excess mortality. Regardless of etiology, lung transplant recipients face a 6.5-fold increase in mortality when diagnosed with lung cancer.
These findings have a few important implications. First, a patient’s individual risk of developing lung cancer in a native lung may need to be included among the many other factors that are considered in the decision to perform a bilateral versus single lung transplant. Second, consideration should be given to more rigorous post-transplant lung cancer surveillance particularly among those receiving a single lung transplant, though it is unclear whether this strategy will improve survival of those diagnosed with cancer.
Dr. Valapour is Director of Lung Transplant Outcomes for the Respiratory Institute and Senior Staff for Lung Transplantation for the U.S. Scientific Registry of Transplant Recipients.
Feature image: H460 non-small cell lung cancer cells were exposed to the antitumor drug cisplatin after autophagy inhibition. The image shows the H460 cells (in green) showing changed staining intensity after inhibition of autophagy. The small bright green bodies are likely to be micronuclei. Autophagy represents a response to chemotherapy and radiation that may be one component of resistance to therapy. Source: NCI Visuals Online. Creator: David A. Gewirtz, Tareq Saleh
Advertisement
Advertisement
First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses
Global R&D efforts expanding first-line and relapse therapy options for patients
Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels
A case study on the value of access to novel therapies through clinical trials
Findings highlight an association between obesity and an increased incidence of moderate-severe disease
Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456
Key learnings from DESTINY trials
Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients