Recurrence-free survival possible, but explain the risks
By Edward Benzel, MD, and Ajit Krishnaney, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
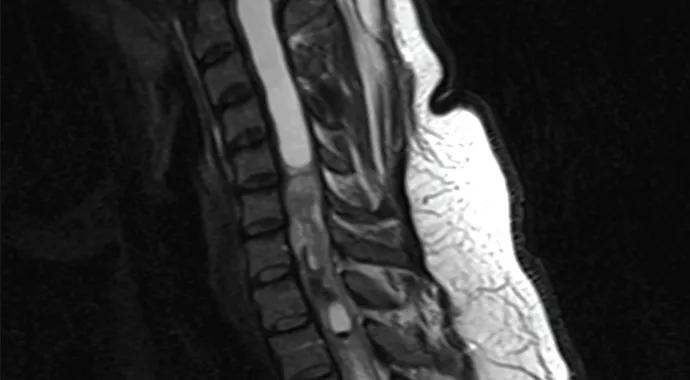
Sometimes life comes at our patients fast. Consider Kristen, a young lady who sought care at Cleveland Clinic’s Center for Spine Health a few years ago, when she was 28. Life was quite good for Kristen: She had married Nick in 2009, and they shared dreams of having a family and building a fulfilling life together. Her zest for life was palpable. Suddenly, however, her world began to collapse. First she had a miscarriage eight weeks into her first pregnancy. Then she had a skin lesion removed that proved to be malignant melanoma. Throughout all this, she was experiencing escalating neck pain, which she largely ignored because of all her other stressors. As the pain progressively worsened, she developed problems with balance and coordination. MRI of her spine revealed yet another problem — an intramedullary cervical spine tumor (i.e., within the substance of the spinal cord; Figure 1).
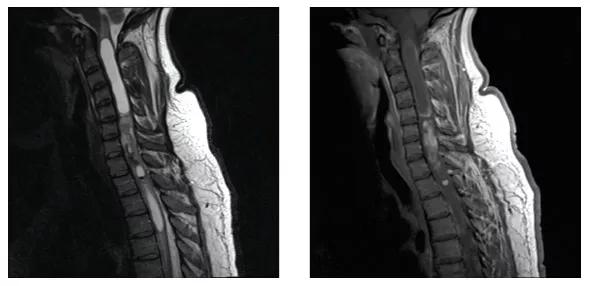
Figure 1.Spine MRIs showing the intramedullary cervical spine tumor.
This newest, and perhaps most challenging, of her problems forced Kristen to confront her mortality. Her expectations of a long and productive personal and family life had already been threatened by the miscarriage and her melanoma diagnosis. While it seemed as though her melanoma was cured by surgery, she was now confronted with this new diagnosis and the many risks associated with removing a tumor from the main corridor ‒ the spinal cord ‒ connecting her brain with the environment in which she lived.
Kristen voiced a litany of concerns and questions: “Holy cow! This tumor is inside my spinal cord?” “I have sooo many other problems.” “Why me?” “Where did this come from?” “How did it get so big with so few symptoms?” “Is it malignant?” “Can I be cured?” “How in the world do you take this out without paralyzing me?”
Advertisement
“Kristen, these are all great questions. In fact, they are very similar to those asked by nearly all patients who have this problem. Let’s start by addressing ‘Why me?’ Simply stated, bad luck ‒ particularly considering your miscarriage and your diagnosis of a malignant skin tumor. No one knows why or how these tumors begin or grow. The good news is that your spinal cord tumor is likely a benign tumor. However, it is situated in a very bad location: the cervical spinal cord. Since it is benign, it grew slowly ‒ very slowly. Likely, your spinal cord adapted to the gradually expanding tumor over time. That’s why you had so few symptoms before this large tumor was diagnosed. We must emphasize that this tumor is not malignant. How do we know? Well, if it were malignant, a tumor of this size would have grown rapidly and not allowed the spinal cord to adapt gradually. If it were malignant, Kristen, you would be paralyzed.
“Kristen, as few as two to three decades ago, neurosurgeons did not operate on patients with spinal cord tumors of this kind (intramedullary). Then, a few surgeons began successfully removing such tumors. Today these tumors can be resected (removed), often with cure. These operations are very risky, however. They involve an incision in the spinal cord followed by tumor removal. The ultimate success is related to multiple factors, the most important of which may be tumor type. Your tumor is likely benign and resectable, but it’s not without substantial risk, including the possibility of developing weakness in your arms or legs, loss of sensation over your body, or loss of bowel or bladder function. You could become dependent on a ventilator or even have complete paralysis, like that experienced by Christopher Reeve. Other risks include medical complications associated with any surgery, such as heart attack, stroke, blood clots in the legs or lungs, wound infection, the need for additional surgery or even death, to name just a few. The tumor type dictates its resectability and the potential for cure.”
Advertisement
Kristen absorbed the information and sought counsel from family and friends. After much discussion, she decided to have surgery. Two intraoperative photographs of the surgical bed after resection are shown in Figure 2.
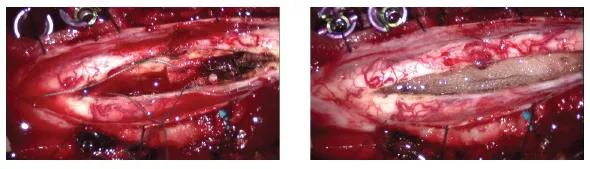
Figure 2. Intraoperative photographs of the surgical bed after resection.
The surgery was uneventful, but Kristen had a challenging postoperative course. As is often the case with intramedullary cervical spine tumors, she was substantially worse neurologically after the surgery. In fact, most patients do not achieve a level of function that is comparable or superior to their preoperative level. Most postoperative patients, like Kristen, experience a moderate to significant decline in function. Kristen lost the ability to walk normally for several weeks, but she gradually improved over six months to her normal baseline level of function. Postoperative MRI demonstrated complete resection of the tumor, without evidence of recurrence at two-year follow-up (Figure 3). The X-rays in Figure 4 show spinal implants required to stabilize the spine after surgery.
Figure 3.Postoperative MRIs showing complete resection of the tumor.

Figure 4.Postoperative X-rays showing spinal implants to stabilize the spine after surgery.
In spite of Kristen’s string of bad luck, she prevailed. Six months after surgery, she achieved a neurological outcome that was near normal ‒ a truly remarkable recovery. During this time frame, however, a second pregnancy ended in another miscarriage. Regardless, Kristen and Nick demonstrated courage and fortitude. She recently gave birth to her daughter, a wonderful reward for all her trials and tribulations.
Advertisement
“It’s sobering to think that 25 years ago, I likely would have been relegated to a treatment course that ultimately would have led to a fatal outcome,” Kristen says. “Surgery can be curative, and I am glad to have chosen the surgical route. It simply has made it all worthwhile.”
Dr. Benzel is Chairman of the Department of Neurological Surgery and a spine surgeon in the Center for Spine Health. His specialty interests include spinal neoplasm.
Dr. Krishnaney is a spine surgeon in the Center for Spine Health, whose specialty interests include spinal cord tumors.
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients