Universal testing could reduce expected costs compared to EGFR single gene testing
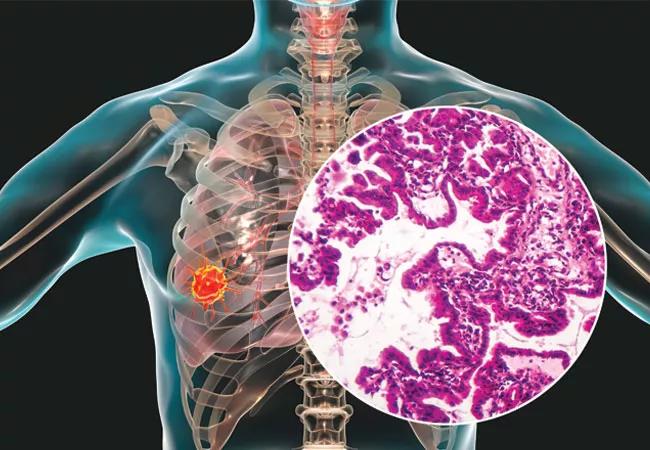
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e734dd90-4235-4c52-9f61-3af82d41b561/23-CNR-3809432-CQD-Hero-650x450-lung-adenocarcinoma_jpg)
lung adenocarcimoa
Comprehensive genomic profiling is an effective means to identify driver alterations and to speed the time-to-treatment at recurrence of early-stage lung adenocarcinoma, according to a recent study published in the Journal of Thoracic Oncology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Up to 70% of patients with non-small-cell lung cancer face disease recurrence after resection. The study found that for patients with targetable alterations, there is a clinical benefit to having broad genomic profiling information before relapse occurs.
In a study of 6,697 patients with lung adenocarcinoma who underwent surgery between 2011-2021, broad testing led to a faster rate of targeted treatment at the time of recurrence with metastatic disease. Additionally, by identifying patients with genomic alterations that do not respond to immunotherapy, there is the potential to enable those patients to avoid futile therapies and associated toxicity. The study estimated that avoidance of immunotherapy in those cases could reduce anticipated costs by $1,497.23 per patient in comparison to EGFR testing.
Broad genomic testing is routine for advanced lung adenocarcinoma, due to the availability of an ever-expanding array of targeted agents, but currently only one in five patients with early disease receive the benefits of such testing. “From a clinical standpoint and from an economic standpoint, it makes sense to perform broad testing for all markers, even in early-stage patients,” explains Nathan Pennell, MD, study co-author and an oncologist with Cleveland Clinic’s Taussig Cancer Institute.
Using a real-world clinicogenomic database, the researchers studied deidentified health records of patients with lung adenocarcinoma who underwent tissue comprehensive genomic profiling. They then used a probabilistic decision tree to estimate the financial implications involved with avoiding immunotherapy for the subset of those patients with programmed death-ligand positive (PD-L1+) lung adenocarcinoma as well as an ALK, ROS1 or RET driver.
Advertisement
In 1,320 of the 6,697 cases, comprehensive genomic testing was performed before the disease advanced, and in 847 of the cases, comprehensive testing was ordered prior to advanced diagnosis. Patients who had comprehensive testing results obtained before recurrence had less time between recurrence and the start of subsequent treatment (median 3.6 vs. 6 weeks).
Beyond this study, definitive data has shown that patients with EGFR mutations do not generally respond to immunotherapy, and a new phase 3 study found that adding the epidermal growth factor receptor tyrosine kinase inhibitor osimertinib in the adjuvant setting significantly improves survival in these patients. “We can extrapolate from stage 4 settings that immunotherapy is ineffective for patients with lung adenocarcinoma who are ALK, ROS1 or RET positive,” explains Dr. Pennell. “Broad testing will spare those patients the risk of side effects from immunotherapy as well as the potential expense.”
“There’s little doubt in my mind that within a decade, patients with lung cancer will have access to adjuvant targeted treatments for all types of mutations, so the need for this testing is going to happen,” says Dr. Pennell. “This study demonstrates that we should be performing comprehensive genomic testing now. If everyone was tested, there would be an additional up-front cost but ultimately it will reduce overall healthcare costs by avoiding treatments known to be ineffective in certain patients.”
Advertisement
Advertisement
First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses
Global R&D efforts expanding first-line and relapse therapy options for patients
Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels
A case study on the value of access to novel therapies through clinical trials
Findings highlight an association between obesity and an increased incidence of moderate-severe disease
Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456
Key learnings from DESTINY trials
Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients