Case illustrates challenges of brain tumors identified during pregnancy
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A case involving a patient diagnosed with a brain tumor late in her pregnancy highlights strategies for managing such challenging situations.
A 34-year-old patient, 27 weeks into her first pregnancy, was admitted to the obstetric unit of Hillcrest Hospital, a Cleveland Clinic hospital, for observation. She reported experiencing persistent nausea, vomiting and severe headache with intermittent blurry vision. The headaches had begun several weeks before admission and were becoming progressively worse.
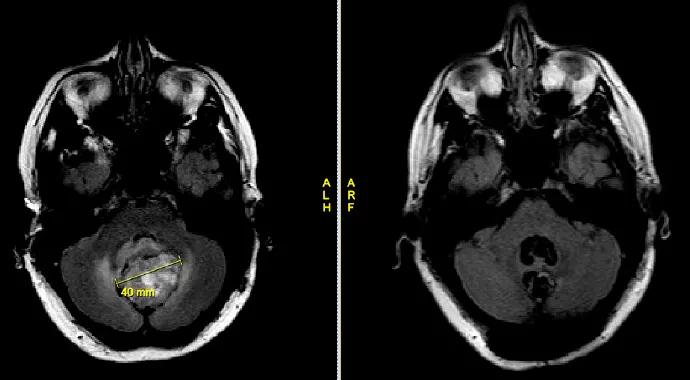
An MRI revealed a large cerebellar hemorrhagic mass with resultant obstructive hydrocephalus. She was then transferred to Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center for further care.
A consult by the Department of Maternal-Fetal Medicine noted the many risks associated with premature birth, including respiratory distress, intraventricular hemorrhage and infection. Delivery at this point in the pregnancy would require a prolonged stay in the NICU. Thus, the report recommended prolonging the pregnancy — if it could be achieved safely for the patient and her baby.
According to the report, if the patient were late preterm or term (after 36 weeks), premature delivery might have been recommended, but only after a diagnosis was made. Without a diagnosis, delivery could be dangerous. If this were an intracranial pathology with increased risk for bleeding, intervention prior to delivery would be recommended, since delivery itself could lead to hemorrhage and rupture of many vascular lesions caused by the massive volume shifts that occur in the peripartum period.
Advertisement
In addition, advised by the neurosurgery team that the patient was facing a risk of neurologic decompensation in the near future because of the size of the tumor and hydrocephalus, Maternal-Fetal Medicine recommended a planned surgical intervention after further imaging. The report noted that the patient should not be in a prone or flat supine position, but added that a lateral, left-tilted or upright position would be acceptable.
Based on the size of tumor and the presentation with increased intracranial pressure, the neurosurgery team determined it was not safe to wait to perform surgery until after term delivery. Thus, we decided to proceed with surgery to remove the tumor two days after the patient was admitted and after pre-operative optimization was performed.
We performed the surgery with the patient in a sitting position, in accordance with the consult. Maternal-Fetal Medicine staff monitored the fetus throughout the procedure, which took approximately 5 to 6 hours. The patient woke up well from surgery, and no fetal distress was detected during the perioperative period.
A postoperative MRI showed complete resection of the tumor. Pathology revealed the tumor was benign, and no postoperative radiation or chemotherapy would be required. The patient went home after a few days and delivered a baby girl two months after surgery, in her 36th week of pregnancy, after premature rupture of membrane. Both the patient and the baby are doing well.
The management of patients with brain tumor discovered during pregnancy poses difficult challenges from various perspectives. Appropriate imaging may not be feasible because of potential risk to the fetus; in this case a decision was made not to do contrast-enhanced MRI. Further challenges arise in terms of prioritizing treatment of the tumor versus continuing the pregnancy.
Advertisement
Some tumors need to be treated as soon as possible, based upon the size or associated symptoms, which was the situation with this patient. In such cases, we need to consider how close we are to term, and whether we can or should terminate the pregnancy at the same time, or do it before or after brain surgery. For this patient, we were prepared for delivery in case of any fetal distress in the perioperative period. Fortunately, everything went well, and she continued her pregnancy for 8 more weeks after brain surgery.
Dr. Mohammadi is a neurosurgeon at Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center.
Advertisement
Advertisement

First-of-its-kind research investigates the viability of standard screening to reduce the burden of late-stage cancer diagnoses

Global R&D efforts expanding first-line and relapse therapy options for patients

Study demonstrates ability to reduce patients’ reliance on phlebotomies to stabilize hematocrit levels

A case study on the value of access to novel therapies through clinical trials

Findings highlight an association between obesity and an increased incidence of moderate-severe disease

Cleveland Clinic Cancer Institute takes multi-faceted approach to increasing clinical trial access 23456

Key learnings from DESTINY trials

Overall survival in patients treated since 2008 is nearly 20% higher than in earlier patients