Potential uses and pitfalls for pulmonologists
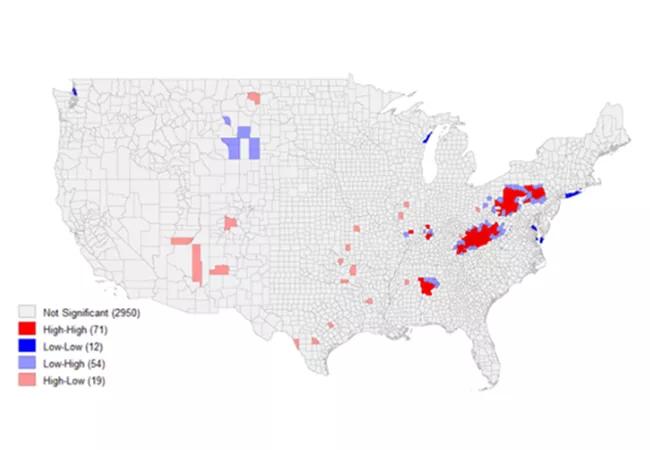
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/484a7e7d-bb19-4ac7-84e0-09fdd6691345/21-PUL-2132163-CQD-Geospatial-Epidemiology-Information-Systems-650x450-map_jpg)
21-PUL-2132163 CQD – Geospatial Epidemiology Information Systems 650×450-map
By Maeve G. MacMurdo, MD, and Wayne M. Tsuang, MD, MHS
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Increasingly we recognize that where patients live, work and spend their time can have a significant impact on their health and well-being. Residential exposure to air pollution has been shown to increase the risk of respiratory and cardiovascular mortality. Neighborhood walkability and safety impact rates of obesity and cardiovascular risk. Toxic emissions may cluster in low-income areas, resulting in increased exposure to potential disease-causing agents.
A better understanding of the relationship between geography, disease risk and disease outcomes enables a health system to deliver targeted population care and enables clinicians to individualize care for patients and communities.
Geographic information systems (GIS) enable mapping and spatial analysis of any patient or population data with location. Due to these capabilities and the novel insights they offer, the use of GIS has been growing rapidly in medical research, public health practice and health system operations. Here we highlight the potential uses of GIS for pulmonologists and researchers, as well as potential pitfalls.
One of the most frequently used GIS techniques in traditional research is cluster or “hot spot” analysis. In this process, the spatial distribution of relevant exposures (or outcomes) is mapped. Spatial analysis techniques help determine patterns of clustering. There are a variety of statistical techniques which can be used to analyze clustering, including global or local indicators of spatial autocorrelation (LISA), or nearest neighbor indexing (NNI). More advanced machine-learning-based cluster analysis is also increasingly utilized. For example, these techniques have been widely used since the beginning of the COVID-19 pandemic for early detection of outbreaks, enabling the rapid mobilization of public health response teams.
Advertisement
GIS also can be used to assess degree and severity of potential exposures within a neighborhood or community, such as assessing the effects of local air pollution on respiratory health. Local level exposures also can be assessed through buffers and interpolation of data across multiple sources.
GIS is increasingly used in combination with traditional statistical techniques to evaluate the relationship between spatial and nonspatial confounders. Geographically weighted regression techniques can help investigate these relationships and provide valuable insights into the relationships between environment, patient factors and risk of disease development.
Rigorous application of GIS requires recognition of its limitations. One of the largest challenges facing researchers utilizing GIS is the need to ensure patient privacy when mapping data. Because GIS links patient data with spatial information, if data presentation is not carefully considered it is possible to extrapolate patient information from visualizations.
To minimize the risk of spatial privacy violations, data is frequently aggregated at the zip code or census tract level. However, both exposures and sociodemographic conditions can vary widely across these larger spatial aggregates.
Cleveland Clinic’s Respiratory Institute is increasingly utilizing GIS in research. In lung transplantation, geospatial mapping is being used to investigate access to transplantation services as well as the impact of environment and community factors on key patient outcomes, such as post-transplantation infection and organ rejection. Researchers in occupational and interstitial lung disease are using GIS to investigate how patients with rare lung diseases access care, and to explore potential relationships between environmental exposures and the risk of developing lung disease.
Advertisement
The environment a patient lives in impacts health, from disease risk to chronic disease management. GIS represents a novel mechanism to explore our patients’ environment and understand the barriers they may face to accessing care. Our aim is to collaborate with community and research partners to better understand these issues and improve care for our patients.
Dr. MacMurdo is a fellow in Cleveland Clinic’s Pulmonary & Critical Care Medicine Fellowship Program. She will join the Respiratory Institute as a staff member in July 2021. Dr. Tsuang is staff in the Respiratory Institute. His specialty interests include lung transplant medicine and critical care medicine.
Advertisement
Advertisement
Volatile organic compounds have potential in heart failure diagnostics
Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients
New program sets out to better support underserved patient populations
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality
Lessons learned from cohorting patients and standardizing care
New tools and protocols to improve care