Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c9207b35-66f4-42f4-a669-3d53ca6c5b2d/23-PUL-4178633-CQD-DM-Revising-US-organ-allocation-lung-transplants_jpg)
lung transplant
Written by Maryam Valapour, MD, MPP
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In January 2023, a 55-year-old woman with interstitial lung disease was listed for a lung transplant. Her lung function had deteriorated despite being on maximal dosing of nintedanib and on presentation she required 8L O2 at rest. Otherwise, she was noted to be short-statured at 4’11” and highly sensitized with a calculated panel reactive antibody of 90% — two factors that would severely limit her access to a donor. In March 2023, her odds of mortality on the waiting list decreased significantly because of the implementation of a new lung allocation system, the Composite Allocation System (CAS) supported by years of research.
The distribution of deceased donor lungs to patients with end-stage lung diseases awaiting a lung transplant is governed by a national lung allocation system. Until March 2023, the allocation of organs was conditional on geographic proximity, clinical measures of donor and recipient compatibility, and finally, a patient’s calculated survival benefit from a transplant expressed by the Lung Allocation Score (LAS). The LAS was empirically derived, but providing patients preferential access to organs within historically defined geographic boundaries without regard for their relative risk of waitlist mortality, or difficulty in accessing a compatible donor was not. Using geographic proximity as the dominant factor in organ allocation was challenged by the medical community due to scientific advances in organ preservation techniques and eventually by patients in the courts.
Advertisement
Cleveland Clinic is home to a group of researchers committed to optimizing the lung allocation system and have been working to fine-tune this system since 2010. As a member of this team and also a Senior Investigator for the Scientific Registry of Transplant Recipients (SRTR), the scientific arm of the US transplant system, I have worked with these teams to devise a system that maximized the survival of waitlisted patients in the new system.
The CAS system combines every consideration in organ allocation including waitlist urgency, post-transplant survival, and candidate biological factors (i.e., blood type, height, degree of sensitization) that affect compatibility and access to the donor pool, and to a much smaller degree, geographic proximity. First, this system aimed to reduce the impact of the geographic proximity of the donor to the candidate in organ allocation. This would allow the sickest candidates or those for whom finding a suitable donor is difficult a broader geographic reach to donors.
Using geolocation tools and driving times, the team identified all active lung transplant programs, donor hospitals and airports nearest each transplant and donor hospital in the United States.1 Then for every recipient-donor pair, travel time was estimated. This analysis showed that further travel was a feasible option for most lung transplant programs. Next came the challenge of choosing how much weight to assign to each of the key determinants of survival on the waiting list in relation to the feasibility of traveling longer distances to procure organs for patients awaiting transplant. Simulation studies presented to the United Network for Organ Sharing (UNOS) lung committee helped policymakers better understand the expected effects of the system, which ultimately decided the components of the system.2
Advertisement
Based on early observations, the adoption of CAS has resulted in lower waitlist mortality for patients awaiting transplant. Medically urgent patients have broader access to donors throughout the U.S. as was the primary intent of the CAS system. This research team is now focused on improving the mortality predictions of the system to rank patients for access to transplant with more precision furthering the goal of maximizing survival of all patients undergoing lung transplant.
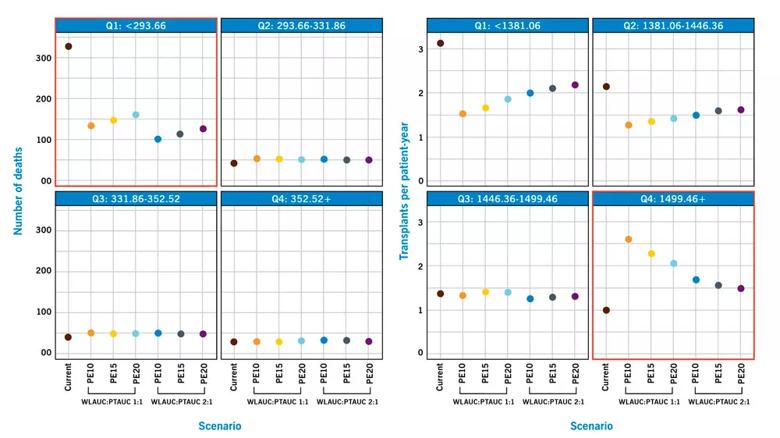
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b1487502-878d-4d31-83f1-2eb7144b13a1/Trade-Offs-Graph_jpg)
Figure Legend. “Trade-offs in survival. Graphs provide point estimates of average minimum and maximum of the range of simulation. Number of waitlist deaths by waitlist area under the curve (WLAUC) quartile is depicted in the left four panels; transplants per patient-year by the posttransplant area under the curve (PTAUC) quartile, in right four panels. These two metrics were compared to show decline in number of deaths in WLAUC quartile at the highest risk of death (Q1) and an increase in transplants per patient-year for all scenarios for those in PTAUC quartile with lowest risk of posttransplant death (Q4) (red boxes). The greatest increase in transplants per patient-year occurred in the Composite Allocation Score scenario where placement efficiency (PE) was given 10% weight with a 1:1 WLAUC:PTAUC ratio.” (Reprinted from American Journal of Transplantation, 22/12, Valapour M, Lehr CJ, Wey A, et al. Expected effect of the lung Composite Allocation Score system on US lung transplantation, 2971-2980, 2022, with permission from Elsevier.)
Advertisement
References
Advertisement
Advertisement
Volatile organic compounds have potential in heart failure diagnostics
Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients
New program sets out to better support underserved patient populations
Lessons learned from cohorting patients and standardizing care
New tools and protocols to improve care
Two NIH grants are looking at developing new antidotes against fentanyl overdose