New guidelines from the American Thoracic Society provide clarity on when to use the test, though some questions remain

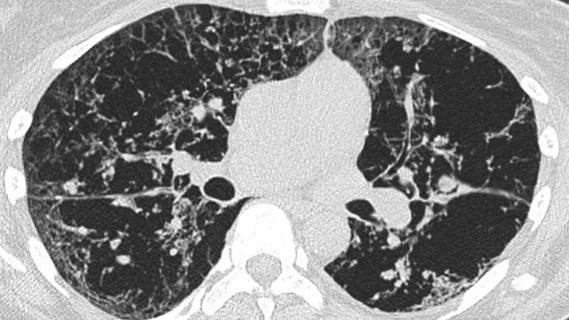
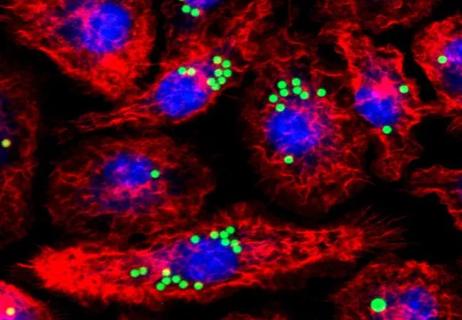
The fractional exhaled nitric oxide test is a simple, safe and non-invasive test to measure inflammation in the airway. But what is the best way to use this test when caring for patients with asthma? That is the question addressed by a new guideline released by the American Thoracic Society.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The fractional exhaled nitric oxide test is a simple test that can be performed in the physician’s office. Patients blow steadily into a tube for a few seconds, and the results are available immediately.
“We’ve known for several years now that nitric oxide was a biomarker for airway inflammation,” says Cleveland Clinic pulmonologist Sumita Khatri, MD. “But there wasn’t a lot of literature available indicating how and when it should be used, or what clinicians should do about high levels. We wanted there to be guidance for clinicians.”
The new guidelines provide clarity by recommending that clinicians use the test to make treatment decisions for patients already diagnosed with asthma. But the guidelines stop short of setting hard-and-fast rules about the levels that should trigger treatment. Instead, they recommend that physicians use their clinical judgment along with the test results when making treatment decisions.
“We found there’s not enough data to support cut-offs,” Dr. Khatri says. “Instead, the results can function as a sliding scale. Each patient is different. If somebody’s nitric oxide is high, but they feel fine, you won’t necessarily treat them. But if their nitric oxide is high and they don’t feel well, that justifies ramping up treatment.”
Dr. Khatri, along with her co-chair, Teal S. Hallstrand, MD, MPH, led an international, multidisciplinary panel of 21 experts tasked with writing the consensus document. Panelists narrowed down more than 2,000 scientific papers to focus on 20 key studies from the past five years that addressed using the exhaled nitric oxide test in treating adult and pediatric patients already diagnosed with asthma.
Advertisement
They found that the test made a difference for two key criteria. First, they found moderate evidence that asthma exacerbations, such as flare-ups, were less frequent in patients when physicians used nitric oxide measurements to guide treatment. “That was very important, because flare-ups of asthma make people miss work, or they don’t feel well and are not fully present. Plus, asthma flare-ups often cause patients to return to their physician for additional care,” Dr. Khatri noted.
Second, having the test results available was associated with lower rates of oral steroid use by patients, another key positive outcome. Interestingly, however, use of the test did not seem to make a difference in whether patients reported that their asthma was under control. There was also no significant difference in emergency department visits or hospitalizations.
Dr. Khatri notes that the American Thoracic Society will be releasing a pocket card with the new guidelines, with a goal of making the recommendations simple and easy for clinicians to implement. She says more data are needed to determine whether the fractional exhaled nitric oxide test is helpful when making an initial asthma diagnosis or while monitoring a patient’s response to treatment.
“Those other two questions are also very important, and we need more research,” she explains. “We need more rigorous clinical trials — evaluating specific subgroups, such as pediatrics vs. adults, checking nitric oxide levels sequentially and characterizing what type of asthma the patient has — so we can come up with additional and practical consensus guidelines.”
Advertisement
Advertisement

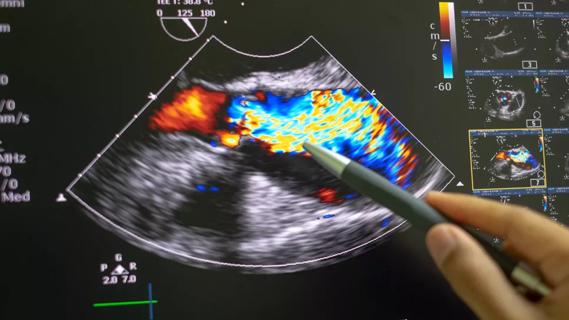
Volatile organic compounds have potential in heart failure diagnostics

Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients

New program sets out to better support underserved patient populations
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality

Lessons learned from cohorting patients and standardizing care
New tools and protocols to improve care