Tips for improving diagnostic accuracy and preventing UTIs
Urinary tract infections (UTIs) are among the most commonly diagnosed infections in older adults, according to Aging Health. For women over age 65, the incidence rate of UTIs is over 10 percent. The incidence rate increases to almost 30 percent for women over age 85. However, these statistics don’t take into account the rate of UTI misdiagnosis in hospitalized older adults, which may be as high as 40 percent.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To improve treatment accuracy and patient outcomes, geriatrician Amanda Lathia, MD, and urologist Howard Goldman, MD, dispel the most common myths about UTIs in older adults and provide recommendations for diagnosis and prevention.
Myth #1: Confusion alone indicates a UTI.
Fact: Older adults have a tendency to experience delirium and confusion, especially if they have any form of cognitive impairment, depression, malnutrition or functional dependency. “Unfortunately, it’s quite common at nursing facilities to check a urine sample at the first sign of confusion,” explains Dr. Lathia. “However, delirium could be caused by a variety of factors — the most common of which is dehydration.”
Myth #2: It doesn’t hurt to check a urine sample.
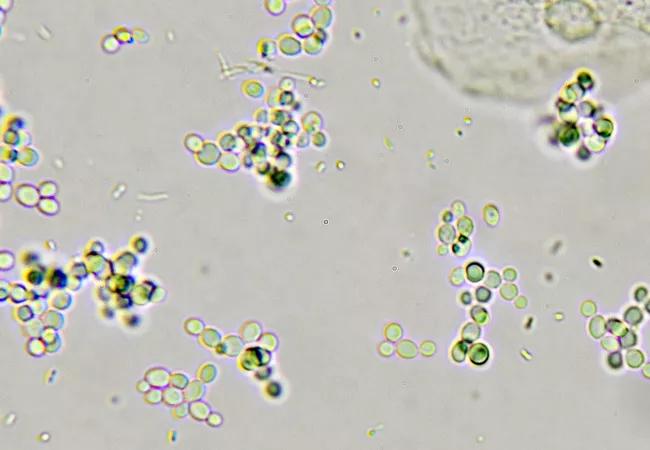
Fact: Problems begin when a doctor checks a urine sample without the patient reporting any other UTI-related symptoms. Many older adults have some bacteria in their urine. “Quite often, this indicates a condition known as asymptomatic bacteriuria, which is characterized by an elevated level of urinary bacteria that doesn’t cause any symptoms,” says Dr. Lathia. According to Aging Health, approximately 6 to 16 percent of women over age 65 and nearly 20 percent of women over age 80 have asymptomatic bacteriuria. For older women living in nursing facilities, the incidence rate ranges from 25 to 50 percent.
“Detecting an innocuous level of urinary bacteria may cause doctors to start an antibiotic without confirming the presence of multiple other UTI signs or symptoms,” explains Dr. Lathia. “This hasty treatment can lead to problems in the future.”
Advertisement
Myth #3: Bacteria in the urine always requires medication.
Fact: Doctors should exercise caution when prescribing antibiotics. If asymptomatic bacteriuria is detected, increasing fluid intake can help restore the patient’s bacterial balance. “If you treat asymptomatic bacteriuria with antibiotics, there’s a good chance that the bacteria in the urine will become resistant to antibiotics, making it challenging to treat a symptomatic UTI in the future,” notes Dr. Lathia. “Antibiotic-resistant bacteria in the urine can increase the patient’s risk of serious complications, including death. Frequent antibiotic use increases the patient’s risk of C. difficile infection.
Myth #4: It doesn’t matter which type of antibiotic you use to treat a UTI.
Fact: Both Cleveland Clinic experts recommend avoiding broad spectrum antibiotics when treating UTIs in older adults. They suggest starting treatment with narrow spectrum antibiotics, which are less likely to lead to antibiotic resistance and problematic side effects. Considering the patient’s health status and other medications, doctors may choose to prescribe trimethoprim/sulfamethoxazole (Bactrim and Septra), nitrofurantoin (Macrodantin or Macrobid) or fosfomycin (Monurol). Cephalexin or amoxicillin-clavulanate may be prescribed to treat uncomplicated lower UTIs.
An accurate UTI diagnosis is especially important for older adults. These patients are usually frail and have a higher risk of experiencing serious UTI-related complications, including hospitalization, delirium and death. Older adults also tend to have comorbid illnesses, which can increase their risk of developing a UTI and display symptoms that are also characteristic of a UTI. When UTIs occur in older men, which is less common, they’re usually caused by a bladder obstruction that should typically be treated by a urologist. Thus, an inaccurate diagnosis could mask a serious underlying problem.
Advertisement
According to Dr. Lathia, the key to an accurate UTI diagnosis is communication. If a UTI is suspected, take the time to discuss symptoms with the patient and/or the caregiver. To confirm a symptomatic UTI, the patient should have a positive urine culture and at least two of the following symptoms:
According to Dr. Goldman, there’s no shortage of old wives’ tales about UTI prevention. For example, cranberry juice/extract is commonly used to prevent UTI recurrence. Probiotics have also become popular for restoring the healthy bacteria in the bladder. “According to the Cochrane Library, there isn’t enough medical research to support the efficacy of either cranberry juice or probiotics in preventing UTIs,” notes Dr. Goldman. “However, their medical benefits cannot be ruled out completely.”
The following strategies can help promote urinary tract health in older adults:
In addition, D-Mannose is a relatively new supplement that is being studied for its potential ability to prevent UTIs while causing few side effects. According to Dr. Goldman, D-Mannose sticks to the receptors in the bladder that would normally attract E. coli, the most common bacteria that causes UTIs. By sticking to these receptors, D-Mannose helps prevent E. coli from staying in the bladder, which may help reduce the risk of UTIs. D-Mannose works similarly in the bowels and is thought to prevent pathologic bacteria from colonizing the gastrointestinal tract, which is where the bacteria that cause UTIs in women may originate.
Advertisement
Advertisement

Pilot study confirms feasibility of conducting additional research on the novel treatment

Longer hospitalization does not mean a safer, faster recovery for patients age 70+

Structured data helps identify older adults at risk for poor outcomes, defines patients who require more comprehensive assessments

Self-administered tool can be completed in 10 minutes in waiting room

Social prescribing turns leisure activities into good “medicine”

A large geriatric study aims to find the answers

Analysis underscores how telehealth can help pinpoint elder abuse