Further studies evaluating the use of pulmonary vasodilators in patients with more severe illness are needed
By Shahnawaz Amdani, MD, and Kenneth Zahka, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
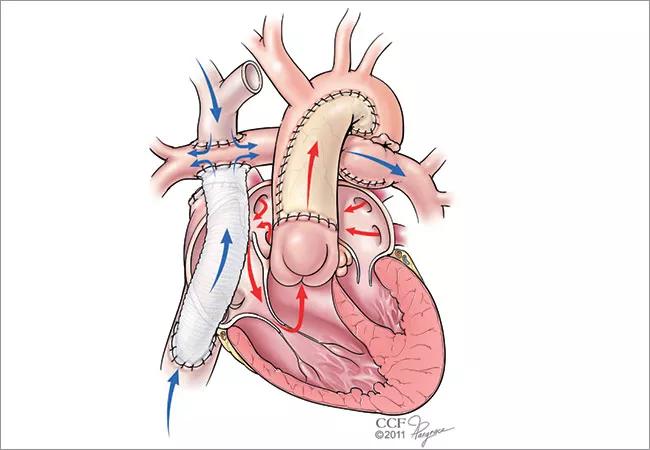
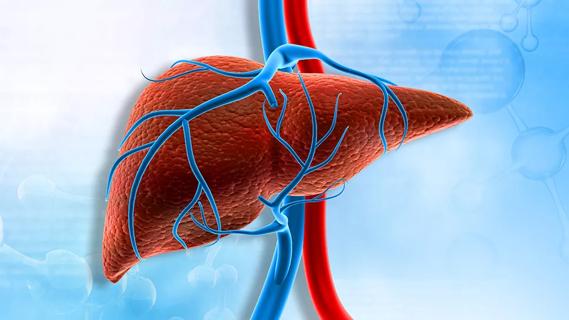
It is becoming increasingly evident that the long-term issues encountered in Fontan patients are secondary to long-standing elevations in central venous pressure (CVP) and diminished cardiac output (CO). In this physiology, pulmonary vascular resistance (PVR) is an important determinant of both upstream (CVP) and downstream (CO) effects.1 Hence, modulation of PVR can have important effects in these patients.
To that end, there are now a few studies that have evaluated different classes of pulmonary vasodilators in Fontan patients: (a) phosphodiesterase (PDE) 5 inhibitors, such as sildenafil;2-7 (b) endothelin receptor antagonists, such as macitentan and bosentan;8,9 and (c) Iloprost, a synthetic prostacyclin analogue.10
Studies using a endothelin receptor antagonists in Fontan patients have shown a reduction in PVR,8 improvement in cardiac index8 and exercise parameters (oxygen uptake, oxygen pulse, anaerobic threshold and exercise time).8,9 Use of Iloprost has also been shown to result in improvement in peak oxygen uptake in Fontan patients. Interestingly, Iloprost led to improvement in all nine (100%) patients who had VO2 <30 ml/kg/min, suggestive of severe exercise limitation, as compared with three out of six (50%) patients who had VO2 >30 ml/kg/min.10
Studies using sildenafil have shown a reduction in PVR and pulmonary resistance index3-5 and improvement in myocardial performance index,6 cardiac output/index,4,5,7 exercise parameters (six-minute walk test distance, oxygen uptake and ventilator efficiency)2,3,7 and NYHA functional class.3
Advertisement
The Fontan Udenafil Exercise Longitudinal (FUEL) trial evaluated the effect of udenafil, a long-acting PDE5 inhibitor, on exercise performance and other cardiovascular and functional outcomes over a 6-month period in Fontan patients. This phase 3, international, multi-center trial included 400 patients – 200 in each treatment arm. 11,12
Adolescents (aged 12-18) who had undergone the Fontan procedure were randomly assigned to a treatment group (87.5 mg of udenafil twice daily) or a placebo group. Investigators made several exclusions, including the following:
Also in the FUEL study, hemodynamic assessments (measurement of Fontan pressures, PVR index, transpulmonary gradient [TPG] and cardiac index) were not performed before or after initiation of udenafil.
The authors did not find an improvement in oxygen consumption at peak exercise; however, udenafil use was associated with improvements in multiple measures of exercise performance at the ventilatory anaerobic threshold.12
Advertisement
First and foremost, the patients that were studied in this trial differ from patients in our clinical practice. As Fontan failure specialists at Cleveland Clinic Children’s, we often see patients that have one or many of the exclusions mentioned above.
In our practice, Fontan patients that are put on sildenafil have hemodynamic evidence of increased PVR, severe ventricular dysfunction, worsening New York Heart Association (NYHA) functional class, liver cirrhosis and active protein losing enteropathy or plastic bronchitis. Before we start sildenafil, we meticulously study their hemodynamics to gauge their Fontan pressures, PVR index/TPG and cardiac index. Clinically, patients who have seen maximum benefit in our practice are those with elevated PVR index/TPG and low cardiac index. Hence, unfortunately the FUEL study does not change our day-to-day practice.
As we’ve outlined above, there are various studies using sildenafil with almost all showing some benefit in PVR, myocardial performance, cardiac output, exercise parameters and NYHA functional class. There are other studies using other pulmonary vasodilators showing benefit in this patient population when used in the right cohort. As shown in the iloprost study,10 we suspect a greater degree of improvement would have been seen in Fontan patients with significant exercise limitation (oxygen uptake < 50% predicted for age and gender), a cohort that was excluded in the FUEL study.
The real question for us is: Would the results be different if the inclusion criteria were altered to include the Fontan patients with severe exercise limitation (oxygen uptake < 50% of predicted for age and gender), severe ventricular dysfunction, patients admitted with recent acute decompensated heart failure, those with evidence of abnormal lymphatics (protein losing enteropathy or plastic bronchitis) or cirrhosis? Also are PDE-5 inhibitors of significant benefit only in those with abnormal hemodynamics (elevated PVR index/TPG and low cardiac index)? Future studies that evaluate the use of pulmonary vasodilators in sicker Fontan cohorts — or those with hemodynamic suggestion of elevated PVR — may help answer these questions.
Advertisement
We commend the Fontan patients, their families and the authors of the FUEL study for trying to answer a clinically important question.
Advertisement
Advertisement

Systemic change needed to improve health outcomes for parents and children, say researchers
Rare genetic variant protected siblings against seizures and severe hypoglycemia

Movie has more positive impact than expected, says Head of Adolescent Medicine

Genetic changes are similar between some vascular anomalies and cancers

Expert panel advises a two-tier structure for surgical centers

Our new head of pediatric general and thoracic surgery shares his passion and vision

Basic understanding of condition and treatment is lacking