An interview with Daniel Culver, DO
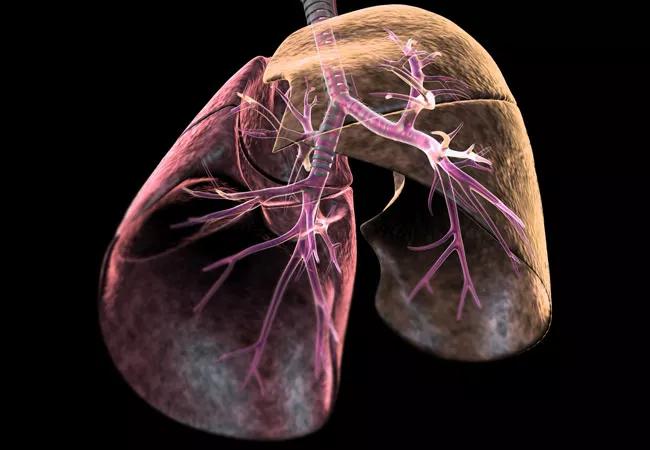
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/36021218-bb3d-48ab-9c6e-2e64aa85ebab/lungs_650x450_jpg)
lungs_650x450
ConsultQD spoke recently with Daniel Culver, DO, about Cleveland Clinic’s Interstitial Lung Disease (ILD) Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
I feel like our ILD program is a large, well-kept secret. Besides having a fully comprehensive, integrated approach to ILD, we are patient focused in a number of ways that many other institutions are not.
For instance, for over 15 years, we have held multidisciplinary discussions (MDD) within our clinic for all of our patients. The MDD involves our entire group of pulmonologists, nurses, our research coordinator, a radiologist and a pathologist. Using an MDD is now the standard of care. When you have a discussion, the decision-making process is much better. In the last couple of months, we’ve opened up our MDD to physicians outside of Cleveland Clinic. And when their patients come to us, we use an integrated scheduling process that allows patients to have multiple evaluations and even procedures in a single visit.
I remember one patient that the MDD helped, a man who was in intensive care doing horribly about fifty miles outside Cleveland. His physician asked us whether cyclophosphamide or other medications would be optimal. When we studied the case, we felt medication would not be helpful but rather an urgent transplant evaluation would be the only option. He was transferred that day and got the transplant the next week. Without the MDD, I’m convinced his condition would have deteriorated so badly that he would have no longer been eligible for transplant.
When community physicians refer patients to us, we want to make sure that we act as partners with them. We want our patients to have a touch point with us and also maintain a relationship with those community-based physicians. That’s the person who will see them if they have a problem after they receive care here. Still, we stay involved in their care through a HIPAA-compliant virtual visit platform. All the patient’s lab results, breathing tests and radiology reports and images can be uploaded into the system for us to see.
Advertisement
The virtual visits can spare patients from travel, especially older patients who may not want to navigate a larger center.
But the virtual approach isn’t for everybody, so many of our physicians and advanced practice providers spend some time working in the community, away from the main campus. I work one day a week at a satellite campus about 30 minutes away.
We use technology to expand the MDD meeting we mentioned above to outside physicians. Every Thursday from 7 to 9 a.m., our ILD pathologist, radiologist and physician discuss complex cases and reach a consensus diagnosis. Physicians outside of Cleveland Clinic can refer an ILD case via email virtualildmdd@ccf.org or telephone call (216.444.3613), and then use a virtual platform to join the discussion about their patient. With this platform, the participants can see the radiologic and pathologic images and video conference with our team in real time.
Today, there are two FDA-approved treatments for idiopathic pulmonary fibrosis (IPF), the most common form of ILD, which has a worse prognosis than most cancers. It’s got an average survival after diagnosis of about three or three-and-a-half years. In fact, more people die from IPF than from breast cancer.
Looking back about three years, the prevailing strategy was to treat IPF patients by treating inflammation. We used drugs like prednisone and azathioprine that were probably harming the patients.
Two years ago, we got two medications for IPF, pirfenidone and nintedanib. But nobody thinks they are the last answer in IPF. Now we are starting to study biologics, small molecules and other therapies that are precise and targeted. These will become the next generation of antifibrotic drugs. We are conducting several clinical trials studying these and other therapies.
Advertisement
Dr. Culver leads the Respiratory Institute’s ILD Clinic.
Advertisement
Advertisement
Volatile organic compounds have potential in heart failure diagnostics
Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients
New program sets out to better support underserved patient populations
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality
Lessons learned from cohorting patients and standardizing care
New tools and protocols to improve care