Efficient procedures with essentially scarless results are achievable

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Minimally invasive cholecystectomy has become the gold standard for gallbladder removal in adults and children. In an effort to improve cosmesis and reduce postoperative pain, single-incision techniques have been developed in recent years. These operations require placement of an umbilical multichannel port or an umbilical incision big enough to accommodate multiple laparoscopic instruments. Though umbilical single-incision procedures have proved safe and effective in children, the use of multichannel ports is not optimal for small children due to the relatively large incisions they require for placement.
In 2010, surgeons in Cleveland Clinic Children’s Department of Pediatric General Surgery began to investigate how established single-port and single-incision approaches to cholecystectomy might be refined to reduce associated pain and scarring while maintaining the procedure’s safety and efficacy. To this end, we employed a first-generation operating laparoscope that has demonstrated success in single-port appendectomy. By reducing instrumentation to its bare essentials, we were able to develop a cost-effective procedure that is not inferior to standard laparoscopic technique and results in a short hospital stay and excellent cosmetic results.
This novel procedure utilizes a 10-mm Storz Hopkins® telescope with zero-degree fiber optics and an inbuilt 6-mm working channel. It is inserted into the abdominal cavity (Figure 1) through a 10-mm transumbilical port.
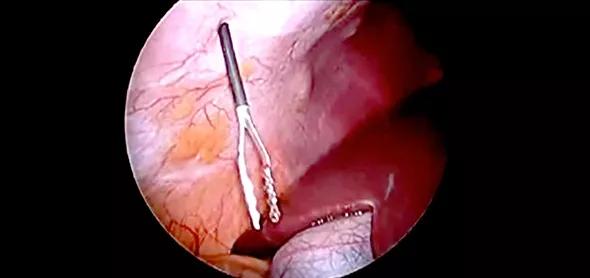
Figure 1. Instrument and trocar placement in the single-port cholecystectomy technique.
Advertisement
Under direct vision, two portless 2.3-mm Clutch Graspers are introduced into the peritoneal cavity through stab incisions in the right subcostal area (Figure 2). The graspers are used to retract and manipulate the gallbladder during the procedure. The cystic artery and ducts are dissected with blunt instruments and hook electrocautery. Low-cost, nonabsorbable Hem-o-lok® clips are used to seal the cystic artery and cystic duct. The gallbladder is separated with electrocautery and removed through the umbilical port site. The umbilical ring is closed with absorbable sutures, and the stab wounds are closed with cyanoacrylate skin glue.
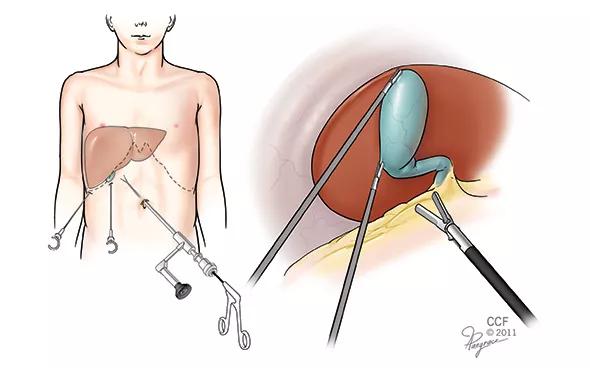
Figure 2. Intraoperative photo showing introduction of the Clutch Graspers into the peritoneal cavity through a stab incision in the right subcostal area.
The zero-degree optic provides sufficient visualization in combination with the use of two holding graspers for patients with standard anatomy.
We recently published our initial experience with this single-port technique in 20 pediatric patients with cholecystolithiasis (n = 13) or biliary dyskinesia (n = 7) over a 14-month period. Patient BMIs ranged from 11.6 to 42.3 kg/m2.
Eighteen patients were treated without incident. Severe pericystic adhesions in two patients required conversion to conventional four-port laparoscopic cholecystectomy. Blood loss in all 20 patients was minimal. No intra- or postoperative complications were experienced.
The average postoperative stay was 24 hours. All patients reported complete resolution of postoperative pain after day 5 and were allowed to resume full physical activity after three weeks.
Advertisement
Since completion of this study, we have expanded the application of this single-port approach to include patients of all sizes and weights with the following forms of benign gallbladder disease:
Our experience through late 2014 includes 124 cholecystectomies with no intraoperative complications. The procedure is now considered the standard approach in our department.
Relative contraindications are few and include the presence of severe scar tissue, patient height of 6 feet or more, and anatomical variants or tissue findings that require better visualization, manipulation with more rigid instruments or conversion to an open approach. The procedure applies standard laparoscopic principles and was quickly adopted by surgeons in training.
In general, we have found that this single-port cholecystectomy technique provides results equivalent to those with conventional, four-port laparoscopic cholecystectomy. Operative times are comparable to, if not shorter than, those with standard cholecystectomy. The use of smaller and fewer skin incisions results in less postoperative discomfort and offers improved cosmetic results.
Preliminary cost analysis suggests that even while this technique maintains the highest standards of safety and outcome, it appears to offer cost savings through reduction of costly operative devices and shortening of operative time and hospital stay.
Dr. Seifarth is a staff surgeon in the Department of Pediatric General Surgery.
Advertisement
Advertisement
Advertisement

Systemic change needed to improve health outcomes for parents and children, say researchers
Rare genetic variant protected siblings against seizures and severe hypoglycemia

Movie has more positive impact than expected, says Head of Adolescent Medicine

Genetic changes are similar between some vascular anomalies and cancers

Expert panel advises a two-tier structure for surgical centers

Our new head of pediatric general and thoracic surgery shares his passion and vision

Basic understanding of condition and treatment is lacking