Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fbc07cb4-a2c8-41d9-b6ee-baef41ce7a11/16-ORT-2551-Molloy-Hero-Image-650x450pxl_jpg)
16-ORT-2551-Molloy-Hero-Image-650x450pxl
By Robert Molloy, MD; Trevor Murray, MD; and Carlos Higuera Rueda, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Value-based purchasing is fast replacing fee-for-service healthcare. In this new era, measuring quality, providing efficiency and achieving good health outcomes will increasingly determine Medicare payments. Under a new incentive system, the U.S. Centers for Medicare & Medicaid Services (CMS) bundled payment program establishes a spending target for all healthcare services over a single episode of care, defined as everything involved in the episode, such as hospital stay, physician services, outpatient care, home health, post-acute care (PAC) and readmissions.
At Cleveland Clinic Euclid Hospital, we voluntarily joined the Medicare Bundled Payment for Care Improvement (BPCI) total joint replacement program in 2013. Our participation helped us examine how we could provide quality joint surgery and achieve savings across the 90-day bundled episode of care. In this program, Medicare and a participating hospital agree to reimburse an episode of care at a target payment based on the hospital’s fee-for-service history for that episode of care and a goal of 3 percent savings. Surgeons and other doctors benefit from the program if savings are realized or exceeded. If a hospital does not meet the 3 percent goal, it must pay CMS for the loss.
At Euclid Hospital, we’ve come a long way in making bundled payments work since we began in 2013. We identified critical areas that required improvement and recognized that we needed new incentives to drive quality care. We focused specifically on:
Advertisement
We identified a care coordinator to manage care across the continuum. Then, we identified patient comorbidities like diabetes that might make a case more complex and costly so that we could manage them appropriately.
In many cases, we needed to shorten LOS. Before bundled payments, patients expected to be in an institution, whether a hospital or a skilled nursing facility, for a week or more. We had to actively manage patient expectations assuring them that they can go home safely with adequate pain management and home care services as a safety net. As we made these changes, we saw that patients were becoming increasingly comfortable with earlier discharge.
We also adopted evidence-based clinical pathways, or care paths, which are key to optimally managing prehospitalization, inpatient care and PAC. Most deviations from the care path were based on patient criteria, not physician preference.
For a program like this to work, physicians must take ownership of the outcomes. Administration, nursing and other caregivers cannot shift care alone. Integrating best practices within and across disciplines is imperative, and all stakeholders must be engaged.
Implementing care paths helped us realize substantial savings and improvement in quality metrics like readmissions. The total two-year cost saving impact of using care paths for total hip arthroplasty (THA) and total knee arthroplasty (TKA) was $1.65 million. Readmissions declined steadily, both for TKA and THA. For THA, readmissions dropped from 5.8 percent to 4.8 percent in 2014, and to 4.0 percent by 2015, representing a 31 percent decrease in readmissions overall.
Advertisement
Similarly, TKA care paths helped drop readmissions 30 percent, with just 3.2 percent readmissions in 2015. Altogether, the total direct cost savings were $319,400 for declined readmission rate for both surgeries over the 2013 to 2015 period (see Figure).
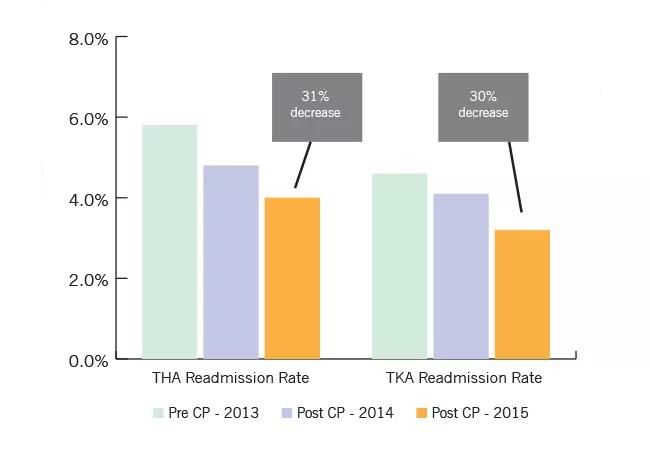
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/363dd096-d37b-4584-8cbf-37c1a8d52281/16-ORT-2551-Molloy-Insert-Image-01-650pxl-width_jpg)
Between 2013 and 2015, safe transitions to home or home health care, rather than a lengthy hospitalization, generated $2.5 million savings. We decreased both our LOS and utilization of PAC dramatically.
Rewarding clinicians who implement these changes with financial or performance incentives is critically important to successfully implementing a bundled payments approach. Based on our early results at Euclid Hospital, we were able to expand the bundled payments program across Cleveland Clinic hospitals to all facilities, except our downtown campus, by 2015. In 2016, we took this further, moving primary, non-complicated cases to regional hospitals and treating only the most complex cases at our main, academic campus.
We believe our results of increased quality, decreased costs and better patient experience are replicable in other regional hospitals and large health systems. Value-based, bundled payments are here to stay, and we must dedicate our best efforts to keeping patients first while adapting to these new models.
Dr. Molloy directs the Center for Adult Reconstruction. Dr. Murray specializes in hip and knee replacement. Dr. Higuera Rueda is staff in the Department of Orthopaedic Surgery.
Advertisement
Advertisement
Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients
How to diagnose and treat crystalline arthropathy after knee replacement
Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network
Reduced narcotic use is the latest on the list of robotic surgery advantages
Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals
Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions