New algorithm recommends optimal approach

By Mostafa Ahmed, MD; Raed A. Dweik, MD; and Adriano R. Tonelli, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Despite significant advances in therapy in the last three decades, pulmonary artery hypertension (PAH) continues to lead to right heart failure and death. Evidence of PAH could be hiding in a common incidental finding on echocardiogram – elevated systolic pulmonary artery (PA) pressure.
Due to the prevalence of false positives, the recommended approaches to address high systolic PA pressure on echo vary from no further investigation to right heart catheterization and, in some cases, referral to a pulmonary hypertension center. We recently proposed a new algorithm for managing high systolic PA pressure echo findings that we hope provides a more accurate, streamlined path to PAH diagnosis.
In short, we don’t know. No consensus has been established on the optimal cutoff for systolic PA pressure echo findings that should trigger further evaluation for PAH.
Our algorithm (below) uses 40 mm Hg as a limit, combined with other echocardiographic variables.
Advertisement
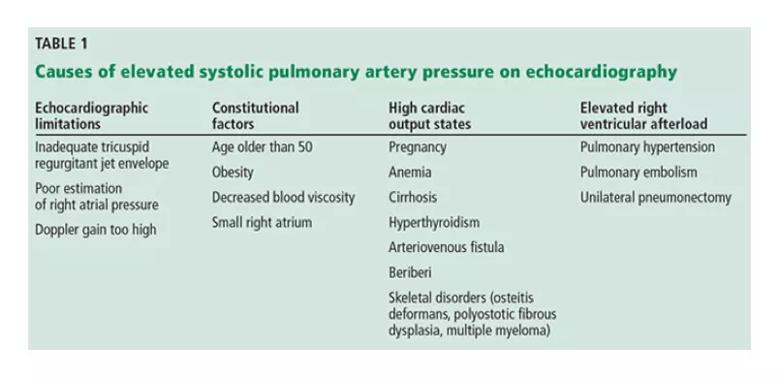
Table 1 shows conditions associated with high systolic PA pressure on echocardiogram. This table demonstrates that the causes of elevated systolic PA pressure on echocardiography are many and not necessarily associated with PAH. Consideration of these other factors must occur before proceeding to right heart catheterization.
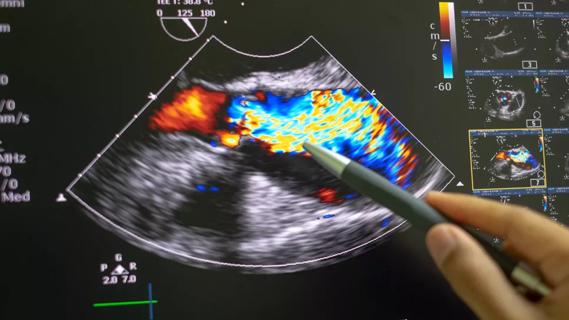
Some echocardiographic features that suggest PAH include a dilated right atrium or ventricle, flattening of the interventricular septum, notching of the right ventricular outflow tract flow and dilation of the main pulmonary artery.
However, echocardiography provides only an indirect measure of systolic PA pressure. Only a right heart catheterization can provide direct evidence of PAH through accurate pressure measurements. Studies comparing measurements during right heart cath with estimated value on echo demonstrate a reasonable degree of agreement between the tests, but a substantial variability. Echo commonly under- and over-estimates systolic PA pressure, with 95 percent limits of agreement ranging from minus 40 mm Hg to plus 40 mm Hg. A difference of plus or minus 10 mm Hg in systolic PA pressure between echocardiography and catheterization was observed in 48 to 51 percent of patients with PAH, particularly in those with higher systolic PA pressure.
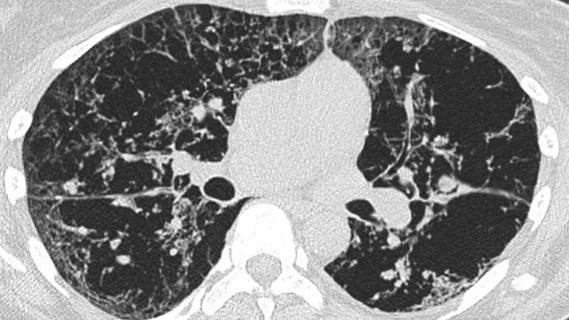
Given the high prevalence of PAH, and the goal of reducing unnecessary procedures, the Fifth World Symposium on Pulmonary Hypertension recommended first considering heart or parenchymal lung disease when an echocardiogram suggests PAH.
Advertisement
Figure 1 details an algorithm we use to investigate elevated systolic PA pressure on echo. In the appropriate clinical setting, if the systolic PA pressure is 40 mm Hg or greater or if other echocardiographic variables suggest PAH, our practice is to proceed with right heart catheterization. If the estimated PA pressure is less than 40 mmHg, the right ventricular size and function are normal and the patient has no diseases associated with PAH, we would not proceed with catheterization.
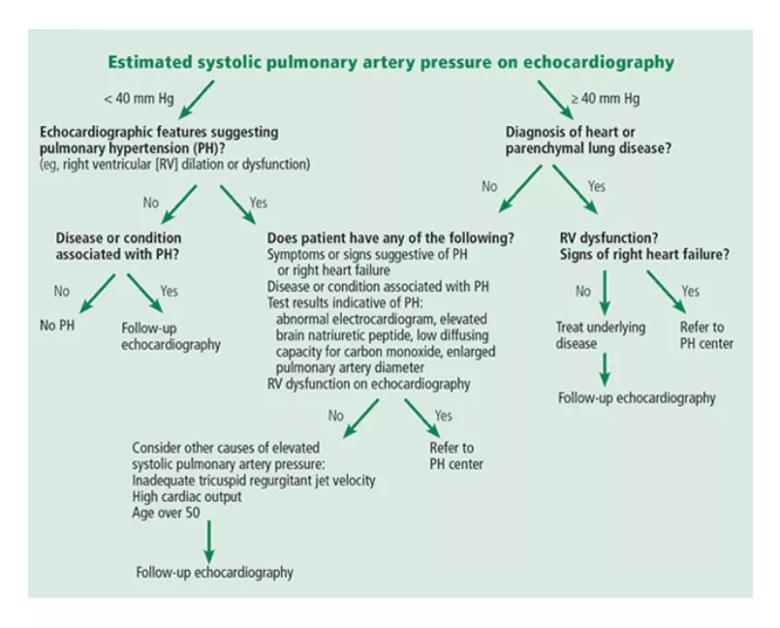
Figure 1. An algorithmic approach to the assessment of systolic pulmonary artery pressure on echocardiography. Adapted in part from Fifth World Symposium on Pulmonary Hypertension recommendations.
In the appropriate context, a high systolic PA pressure on echocardiography suggests PAH, but right heart catheterization is needed to confirm the diagnosis. Since estimating systolic PA pressure with echocardiography has limitations, including false-positive results (predominantly when the pretest probability of PAH is low), care must be taken in both diagnosing and proceeding with additional testing. Our algorithm serves as a useful guide.
Read more about PAH on Consult QD.
What do patients want to know about pulmonary hypertension? View this Cleveland Clinic Online Health Chat with Dr. Tonelli.
Dr. Ahmed is a Research Fellow, Department of Pulmonary, Allergy, and Critical Care Medicine, Respiratory Institute.
Dr. Dweik is Director of the Pulmonary Vascular Diseases Program, Department of Pulmonary, Allergy and Critical Care Medicine, Respiratory Institute.
Advertisement
Dr. Tonelli is staff, Department of Pulmonary, Allergy and Critical Care Medicine, Respiratory Institute.
Advertisement
Advertisement

Volatile organic compounds have potential in heart failure diagnostics

Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients

New program sets out to better support underserved patient populations
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality

Lessons learned from cohorting patients and standardizing care
New tools and protocols to improve care