Increase signals disease progression
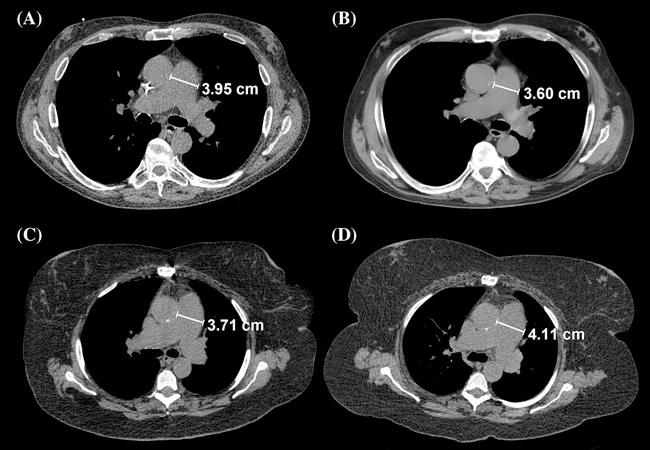
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/cf065fee-8310-4c6d-ac35-015c6ca8569b/Tonelli-CQD-Image-650x450pxl_jpg)
Tonelli-CQD-Image-650x450pxl
Patients with pulmonary arterial hypertension (PAH) often present with dilated pulmonary arteries (PA). The literature says little, however, on variations in size of the pulmonary artery over time, whether such changes track with disease progression and whether or not they predict patients’ long-term survival.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Recently, a group of Cleveland Clinic physicians decided to test whether patients with PAH have PA dilation that worsens over time and whether that is associated with worse outcomes.
“We looked at patients with pulmonary arterial hypertension who had at least two CT scans of their chest done on different occasions,” says Adriano Tonelli, MD, Department of Pulmonary Medicine. “We also reviewed their echocardiograms and six-minute walk tests that were performed at the same time as the CT scan. To our knowledge, this is the first study to assess changes in pulmonary artery diameter over time in patients with PAH.”
Dr. Tonelli and his colleagues studied a cohort of 113 PAH patients of which 28 percent were male and 72 percent were female. The racial breakdown was 77 percent white, 22 percent African American and 1 percent Asian. Finally, the origin of their PAH was 44 percent connective tissue disease, 30 percent idiopathic, 11 percent congenital heart disease, 10 percent portal hypertension, 5 percent heritable and 2 percent associated with anorexigens/toxins.
They found that the main PA diameter increased by at least 1 mm in 40 percent of the patients after 12-month follow up. Overall their data show that time between CT scans was directly associated with the increase in PA diameter. When adjusted by time between scans and difference in slice thickness, three variables were associated with a more pronounced mean PA diameter: a higher PA pulse pressure and lower PA compliance during right heart catheterization, worse RV function on the echocardiograms performed close to the first and second CT scans andhigher right ventricular systolic pressure (RVSP). A decline in the six-minute walk test was also associated with PA dilation.
Advertisement
The researchers found that main PA diameter at baseline was a significant predictor of mortality, when adjusted for difference in time and slice thickness between CT scans, age, gender and PVR. The change in main PA diameter over time was also a significant predictor of mortality when adjusting for the same factors or when adding the diameter of the main PA at baseline, origin of PAH or time from the diagnostic right heart catheterization and initial CT scan of the chest.
“We found that for every 1 mm expansion in the main pulmonary artery, there was a 28 percent increase in mortality,” Dr. Tonelli says.
Change in PA area significantly impacted survival. The median follow-up was 33 months, during which 53 patients (46.9 percent) died and six were censored due to lung transplant. Survival at one and two years was 65 percent and 61 percent, respectively. However, the changes in other determinations such as main PA/Ao diameter ratio, right PA diameter and left PA diameter, were not significant predictors of survival when adjusted for similar variables as used in previous analyses.
Thirteen percent of patients demonstrated a decrease in PA diameter over time. Six had a reduction of at least 1 mm and five of at least 3 mm when CT scans were performed at least 12 months apart. The effect was more prominent in patients with portopulmonary hypertension than in those with idiopathic PAH.
“The reason for the decrease is unclear,” says Dr. Tonelli. “It may be due to reverse remodeling of the pulmonary artery due to improvement in pulmonary hemodynamics and/or decrease in intravascular volume.”
Advertisement
Feature image: Main PA diameter measurement during first and second CT scans of the chest. Panels (A) and (B) correspond to a PAH patient in whom the main PA diameter decreased by 3.5 mm, while panels (C) and (D) showed the axial CT cuts of another PAH patients in whom the main PA diameter increased by 4 mm during follow‐up. Originally published in Respirology.
Advertisement
Advertisement
Volatile organic compounds have potential in heart failure diagnostics
Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients
New program sets out to better support underserved patient populations
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality
Lessons learned from cohorting patients and standardizing care
New tools and protocols to improve care