HDL-C and outcomes in CTEPH
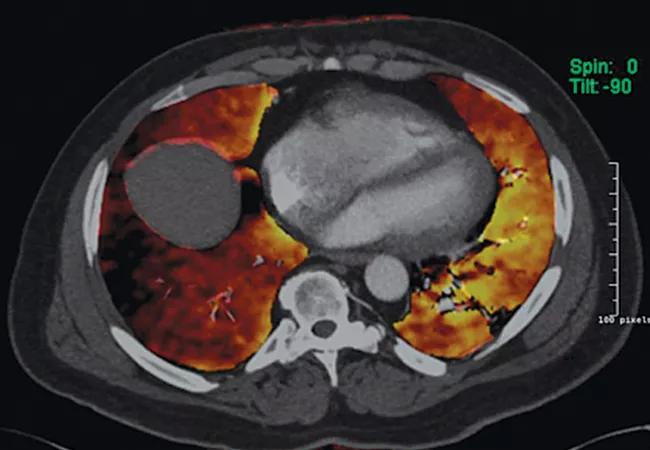
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/77db119c-0a1e-4ba3-ab8a-b505e022ac65/15-PUL-3009-CTEPH-CQD-650x450_jpg)
Chronic Thromboembolic Pulmoary Hypertension Program
By Ghaleb Khirfan, MD, and Gustavo Heresi, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
High-density lipoprotein cholesterol (HDL-C) has various anti-inflammatory, anti-atherogenic, anti-oxidant and anticoagulant properties that improve vascular function. The utility of HDL-C as a biomarker of severity and predictor of survival has been described in patients with pulmonary arterial hypertension (PAH), but no prior study has assessed the utility of HDL-C in patients with chronic thromboembolic pulmonary hypertension (CTEPH). Our recent study published in PLoS One compared the levels of HDL-C in CTEPH patients with those found in PAH patients and controls and assessed the association between HDL-C and markers of disease severity and survival.
CTEPH, which is classified as group 4 pulmonary hypertension (PH) in the updated clinical classification, is a relatively rare sequela of pulmonary embolism (PE), with estimated incidence of 0.57 to 3.8 percent after an episode of acute PE. It is caused by obstruction of the pulmonary vessels and distal small vessel vasculopathy that leads to increase in the pulmonary artery pressure and pulmonary vascular resistance. It has a dismal prognosis without timely surgical intervention, leading to right heart failure and death.
Recent studies have identified HDL-C as a biomarker of severity and predictor of survival in PAH patients. PAH patients were found to have lower levels of HDL-C than controls, with lower HDL-C associated with worse outcomes. Given the results of these studies and the similarity between the small vessel vasculopathy in CTEPH and vascular lesions in PAH, we hypothesized that abnormalities exist in HDL-C levels in CTEPH patients and that HDL-C might be a marker of small vessel disease in these patients.
Advertisement
We studied a total of 90 patients with CTEPH (mean age ± SD: 57.4 ± 13.9 years; female, 40 percent), 69 patients with PAH (mean age ± SD: 46.7 ± 12.8 years; female, 90 percent) and 229 control subjects (mean age ± SD: 56.7 ± 13 years; female, 47.6 percent). HDL-C levels in CTEPH patients were significantly lower compared with control subjects and higher compared with PAH patients (median, interquartile range: CTEPH: 44, 34-57 mg/dl; PAH: 35.3, 29-39 mg/dl; control: 49, 40-60 mg/dl; P < 0.01, for both pairwise comparisons).
Higher plasma HDL-C was associated with decreased prevalence of right ventricular dilation on echocardiography (P = 0.02). There were no other statistically significant associations between HDL-C levels and other markers of disease severity or mortality. In the subset of patients with CTEPH who underwent pulmonary thromboendarterectomy (PTE), higher baseline HDL-C was associated with a larger decrease in pulmonary vascular resistance (PVR) postoperation (R = 0.37, P = 0.049).
In summary, our study showed that HDL-C in CTEPH patients is lower compared with control subjects, but higher compared with PAH patients. Higher baseline HDL-C in CTEPH patients was associated with decreased prevalence of right ventricular dilation on echocardiography and, among those who underwent PTE, a greater decrease in postoperative PVR. These data suggest that plasma HDL-C may be a useful marker of small vessel disease in CTEPH.
Future studies with larger sample size are needed to assess the utility of HDL-C as biomarker in CTEPH and should answer the question of whether changing levels of HDL-C in these patients will impact clinical outcomes.
Advertisement
Dr. Khirfan is a Pulmonary and Critical Care fellow in the Respiratory Institute. Dr. Heresi is staff in the Departments of Pulmonary Medicine and Critical Care Medicine.
Advertisement
Advertisement
Volatile organic compounds have potential in heart failure diagnostics
Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients
New program sets out to better support underserved patient populations
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality
Lessons learned from cohorting patients and standardizing care
New tools and protocols to improve care