Case demonstrates safety in properly selected patient

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy

Audrey Rhee, MD
The robotic approach in pediatric urologic surgery is constantly under scrutiny. This stems from the fact that many reconstructive procedures can be performed in less operative time using an open approach, with similarly small sum-total incisions. Pediatric patients who undergo open urologic procedures rarely remain hospitalized more than two days postoperatively unless they are older and more muscular. Thus, the patient selection and procedure performed must justify the cost and approach in robotic cases.
Here we review the first pediatric robot-assisted partial nephrectomy performed at Cleveland Clinic. The patient, a 9-year-old female, initially presented with epigastric pain. She was ultimately diagnosed with chronic pancreatitis; however, imaging incidentally revealed a complex left upper pole cystic lesion. This 1.1 x 0.8 cm T1 and T2 hypointense, nonenhancing lesion consistent with a renal cyst was in the superior pole of the left kidney. Septations and calcifications were present.
Notably, the patient had a duplex collecting system on the left kidney; however, this was not associated with a dysplastic upper pole or dilated ureter. Nor did it appear to be consistent with a calyceal diverticulum.

Figure 1. Preoperative ultrasound of the left kidney, sagittal view, showing a 1.6 x 1.1 x 0.9 cm cystic lesion in the upper pole. There is increased echogenicity within the periphery which may reflect calcifications.

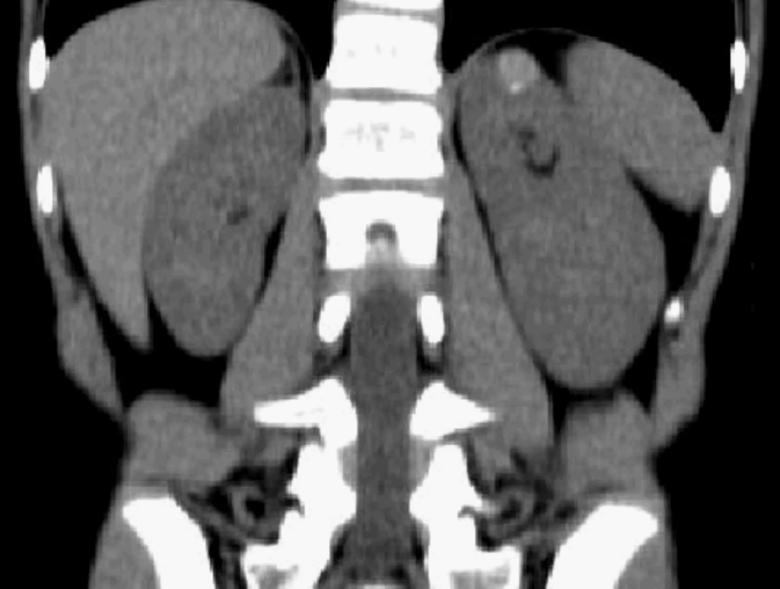
Figures 2 and 3. Preoperative CT scan images, axial and coronal views, showing a 9 x 9 x 12 mm hyperdense (80 HU) round endophytic lesion in the upper pole of the left kidney, with a 3 mm peripheral calcification inferiorly. No layering fluid levels are seen within the lesion.
Advertisement
After extensive counseling, we offered the patient’s parents the options of watchful waiting or excision of the lesion. Given the complexity of the lesion, the parents were interested in pursuing excision but were not keen on an open approach. Our pediatric urology and minimally invasive teams reviewed the patient’s medical imaging and determined that the procedure could be performed robotically.
Retrograde pyelograms confirmed the duplex collecting system and that the upper pole lesion was not merely a dysplastic upper pole. An open-ended ureteral catheter was left in place in the lower pole ureter for identification purposes.
The robot was docked using a 12 mm camera port, 8 mm standard robotic arm ports and a 12 mm assistant port. We carefully defatted the left kidney and dissected the hilum. A laparoscopic ultrasound confirmed our preoperative findings. We applied a bulldog clamp to the renal artery and excised the renal lesion in its entirety. The renorrhaphy was closed in a running horizontal mattress fashion. Total warm ischemia time was 13 minutes.
The patient did well after surgery and was discharged the next day with a stable complete blood count. The pathology report confirmed a benign renal cortical cyst.
The patient obtained a follow-up ultrasound which demonstrated a healthy left kidney with no residual lesions. Two years postoperatively, her images are consistently unchanged. Her small abdominal incisions are well-healed and well-concealed.
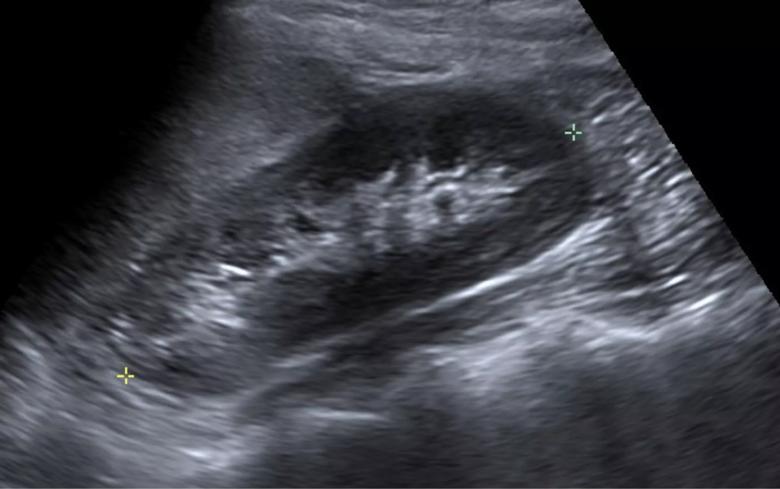
Figure 4. Ultrasound of left kidney, sagittal view, two years postoperatively. Previously noted cystic lesion is not seen at the superior pole, and there is no evidence of hydronephrosis.
Advertisement
Hemi-nephrectomies in this pediatric patient population have been reported. However, blood loss is markedly less in a nonfunctioning upper pole than in a potentially vascular and malignant lesion. Partial nephrectomies are less common and few are managed minimally invasively.
This case demonstrates that in addition to reconstructive procedures such as pyeloplasty or reimplants in the pediatric population, extirpative robotic procedures are also a safe option. Had this child undergone an open approach, her recovery would likely have been much longer, given her age and size. Additionally, her incision would have been much larger.
Proper patient selection is the cornerstone of success in robot-assisted cases.
Dr. Rhee is an associate staff member of Cleveland Clinic’s Department of Urology and of the Center for Pediatric Urology at Cleveland Clinic Children’s.
Advertisement
Advertisement

Systemic change needed to improve health outcomes for parents and children, say researchers
Rare genetic variant protected siblings against seizures and severe hypoglycemia

Movie has more positive impact than expected, says Head of Adolescent Medicine

Genetic changes are similar between some vascular anomalies and cancers

Expert panel advises a two-tier structure for surgical centers

Our new head of pediatric general and thoracic surgery shares his passion and vision

Basic understanding of condition and treatment is lacking