Discovery may lead to novel therapies
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
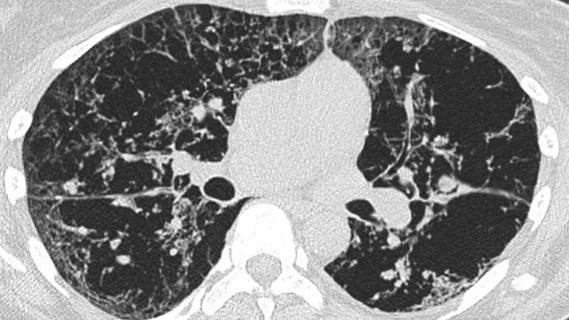
Our laboratory has recently shown that the mechanosensitive, calcium-permeable, plasma membrane ion channel named transient receptor potential vanilloid 4 (TRPV4) plays a role in myofibroblast differentiation and in vivo lung fibrosis1.
The pathogenesis of pulmonary fibrosis depends on soluble factors and a mechanical signal (extracellular lung matrix stiffness). Similarly, effective macrophage engulfment of foreign particles (phagocytosis) requires orchestration of macrophage surface receptors, the particle itself and the extracellular matrix.
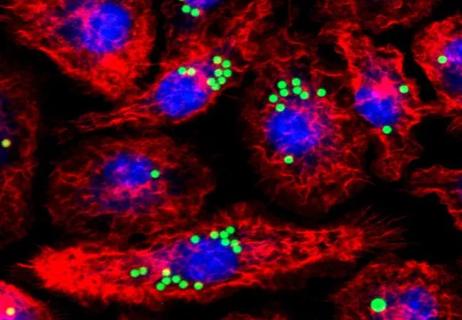
Acute respiratory distress syndrome (ARDS) from an infectious stimulus is a complex process characterized by endothelial and alveolar epithelial injury followed by recruitment and accumulation of inflammatory cells (i.e., macrophages) in the injured alveolus. Macrophages play a key role in lung injury and fibrosis by producing cytokines and other inflammatory remodeling factors. Hence, we sought to determine the role of TRPV4 in clearance of infection by macrophages (phagocytosis) and associated lung tissue injury.
We investigated the role of TRPV4 in integrating the dual signals provided by matrix stiffness and lipopolysaccharide (LPS), an important constituent on the surface of gram-negative bacteria, to control macrophage phagocytosis and cytokine production for host defense and resolution of lung injury.
In work recently published in the Journal of Immunology, we showed that inhibition of TRPV4 by pharmacologic agents or downregulation/deletion of TRPV4 resulted in almost complete blockage of LPS-stimulated macrophage phagocytosis in vitro and in vivo in a matrix stiffness-dependent manner. Moreover, TRPV4 mediated the LPS signal to release anti-inflammatory/ pro-resolution cytokines in macrophages.
Advertisement
Taken together, these results implicate the mechanosensing channel, TRPV4, in the pathogenesis of gram-negative bacterial pneumonia and resolution of associated acute lung injury by integrating the LPS and the matrix stiffness signals for macrophage phagocytosis and pro-resolution cytokine release.
Pharmacologic agents targeting TRPV4 are currently under development and in Phase I clinical trials. Successful targeting of TRPV4 channel activity may lead to therapeutic approaches to treat bacterial pneumonia and associated ARDS.
Dr. Scheraga is an associate staff physician at the Respiratory Institute and holds a secondary appointment in the Lerner Research Institute Department of Pathobiology. For more information contact Dr. Scheraga at 216.444.4429 or scherar@ccf.org.
Advertisement
Advertisement

Volatile organic compounds have potential in heart failure diagnostics

Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients

New program sets out to better support underserved patient populations
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality

Lessons learned from cohorting patients and standardizing care
New tools and protocols to improve care