Tips for primary care physicians from vascular medicine specialist Leslie Gilbert, MD

A: When taking a history, I typically ask the following:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The BMI is key because obesity may play a significant role in edema. A full examination with the patient in a gown, lying flat on an exam table, is important to assess for:
Also, observing patients’ gait shows whether the bellows-like calf muscle pump is activated.
It’s important to distinguish a volume-mediated from a pressure-mediated process. Compression garments will help if pressure is the problem.
Controlling edema prior to fitting patients for compression garments is critical. The products’ comfort, ease of placement and removal, and cost will all factor into patient compliance. Sending a patient off with a prescription without further insight is likely to result in failure and frustration.
A lymphedema specialist or clinic can provide expertise in guiding patients through this process by:
Advertisement
Some patients may prefer Velcro compression garments for their ease of application and ability to help them maintain independence. Other patients may need additional night-time compression, but that decision is best made after consultation with a lymphedema specialist.
Dr. Gilbert, a staff physician in the Department of Vascular Medicine, is also on staff in the Wound Healing Center at Cleveland Clinic’s South Pointe Hospital.
Advertisement
Advertisement

OMT may be right for some with Graves’ eye disease

Perserverance may depend on several specifics, including medication type, insurance coverage and medium-term weight loss

Integrate climate-related health information and counseling into your practice
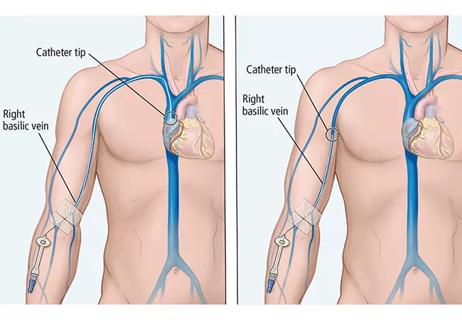
Physicians discuss a specific case example, and PICC pros, cons and alternatives

A snapshot of the 2020 GINA report

A review of available interventions

Abstinence from combustibles, dependence on vaping

An historical view of the disease