Making lung transplant an option in complex cases

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7cdfc643-8fff-4afa-bd84-b0e1303368cd/18-PUL-5758-Budev-Hero-Image-650pxl-width_jpg)
18-PUL-5758-Budev-Hero-Image-650pxl-width
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 44-year-old woman with a history of myelodysplastic syndrome refractory to medical therapy underwent an allogenic bone marrow transplant in December 2017. The patient did well post-transplant until the spring of 2018, when she began to notice a nonproductive cough and increasing dyspnea on exertion.
In May 2018, the patient presented with acute hypoxemic respiratory failure and was intubated and empirically treated with broad-spectrum antibiotics and high-dose steroids. All microbiologic studies, including respiratory cultures, were negative for infection, including pneumocystis. Echocardiography demonstrated no evidence of an intracardiac shunt accounting for her hypoxemia. A CT scan of her chest showed no evidence of pulmonary embolism, but demonstrated extensive ground-glass opacities.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7cdfc643-8fff-4afa-bd84-b0e1303368cd/18-PUL-5758-Budev-Hero-Image-650pxl-width_jpg)
Chest X-ray before lung transplant.
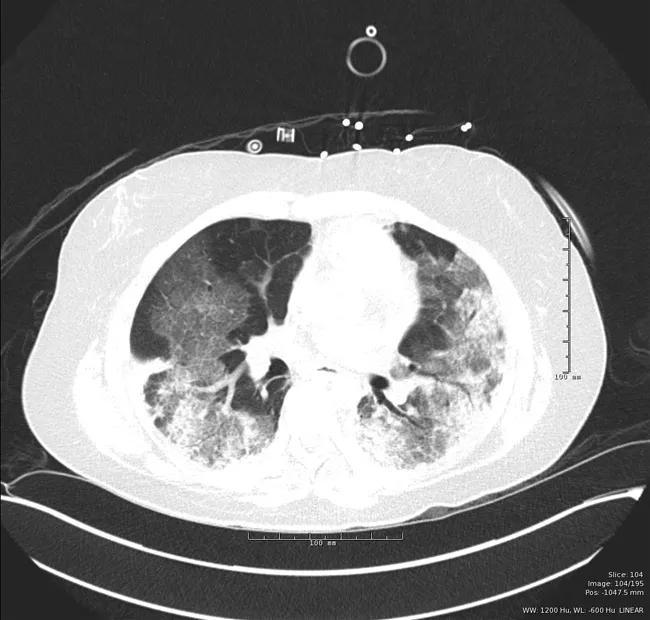
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0010ca79-f188-46db-a947-14041a8bd501/18-PUL-5758-Budev-Inset-Image-02-650pxl-width_jpg)
CT scan before lung transplant, demonstrating extensive ground-glass opacities.
Despite aggressive therapy, the patient’s condition deteriorated, and the patient was emergently placed on venovenous extracorporeal membrane oxygenation (VV ECMO) as a possible bridge to lung transplantation.
The medical and surgical lung transplant teams, in conjunction with the medical oncology and bone marrow transplant teams, discussed in detail the appropriateness of lung transplant listing. It was felt that the patient’s bone marrow transplant had engrafted fully, that the patient was essentially cured of her myelodysplastic syndrome, and that her bone marrow would be able to withstand the myelosuppressive drugs used as part of the immunosuppressive regimen in lung transplant recipients. It also was felt that the CT findings were consistent with idiopathic pneumonia syndrome in the setting of her previous bone marrow transplant and that the likelihood of recovery in the absence of lung transplantation was remote. The decision was made to place the patient on the active waitlist.
Advertisement
The patient was extubated and rehabilitated in the intensive care unit while on ECMO support as she awaited lung transplant. Eleven days later she underwent an uncomplicated bilateral sequential lung transplant and was extubated the next day. The patient was discharged from the hospital to her home two weeks later. Her explant lung pathology did show extensive alveolar damage compatible with idiopathic pneumonia syndrome with no evidence of infection.
At the time of discharge, the patient was ambulatory and on room air with only mild thrombocytopenia on her complete blood count. Her pulmonary function testing and routine chest X-rays continue to improve at each outpatient visit.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1d10ca5d-a504-4026-88cd-2f1299557f46/650x450-Budev-Inset-Image_jpg)
Chest X-ray after lung transplant.
This extremely complex case illustrates the close collaboration among the various transplant, critical care, and consultant teams at Cleveland Clinic and the ultimate willingness of the lung transplant program to offer this option to patients who likely would not be deemed suitable by other programs.
Dr. Budev is the Medical Director of Lung Transplantation and holds the Macon and Joan Brock Endowed Chair for Lung Transplantation at Cleveland Clinic.
Advertisement
Advertisement
Volatile organic compounds have potential in heart failure diagnostics
Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients
New program sets out to better support underserved patient populations
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality
Lessons learned from cohorting patients and standardizing care
New tools and protocols to improve care