Pulmonary thromboendarterectomy prolongs life expectancy
By Gustavo Heresi, MD, Marcelo Gomes, MD, Karunakaravel Karuppasamy, MD, Abraham Levitin, MD, and Nicholas Smedira, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 21-year-old female with a diagnosis of chronic thromboembolic pulmonary hypertension (CTEPH) was referred to Cleveland Clinic for heart-lung transplantation. She was considered not to be a candidate for pulmonary thromboendarterectomy (PTE) due to a large venous malformation in the mediastinum. She was born with a left axillary mass, for which she received no treatment. She reported a one-year history of dyspnea on exertion. Six months prior she had an acute pulmonary embolism. Her dyspnea progressed to functional class III upon presentation in spite of ongoing anticoagulation.
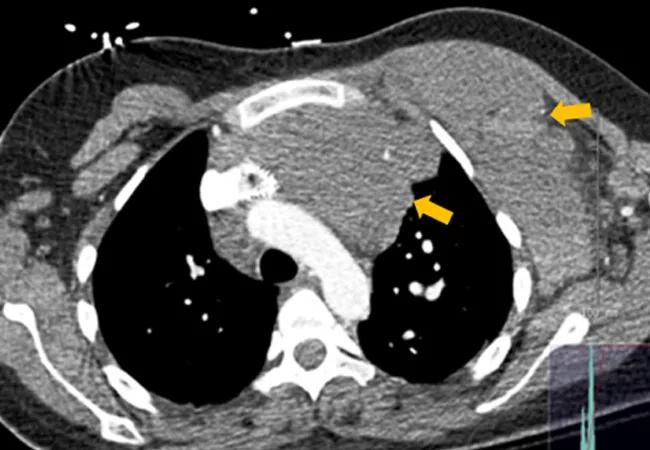
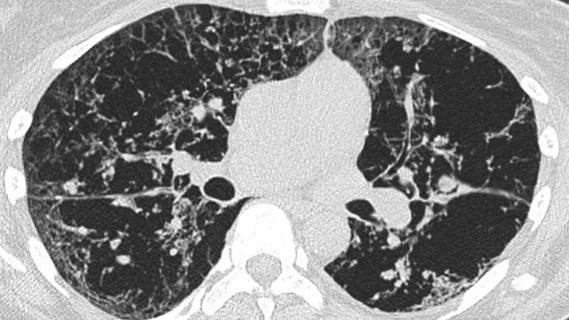
Chest computed tomography (CT) showed a huge venous malformation in the left anterior mediastinum lying immediately behind the sternum, extending across the midline anterior to the thoracic aorta and across the thoracic outlet into the left axilla and chest wall; the mass abutted the right ventricular outflow tract and the main pulmonary artery.
Angiography showed her left axillary vein bifurcated and fed the malformation, which drained into the left innominate and, ultimately, the superior vena cava (SVC). Magnetic resonance angiography additionally depicted thrombosis in the axillary portion of the malformation, and a series of tandem covered stents extending 18 cm from the left axillary vein to the SVC that had been placed at another institution to isolate the malformation from the systemic circulation.
Both chest CT and invasive pulmonary angiography documented central chronic thromboembolic disease. Right heart catheterization demonstrated severe pulmonary hypertension and severely elevated pulmonary vascular resistance.
Advertisement
The patient underwent direct puncture venography of the malformation, which documented minimal early drainage into the mediastinum. Embolization of multiple feeding pathways and of the malformation itself was successfully carried out.
During PTE, the surgeon spent several hours dissecting the mass from the mediastinal structures and mobilizing it both superiorly and to the left side. An incision was made in the thickest portion of the malformation, the clot was extracted and a basket sucker was used to maintain it in a decompressed state.
A complete endarterectomy was performed using 23 minutes of circulatory arrest for the left and 10 minutes for the right side. The patient had an uneventful postoperative course with significant hemodynamic improvement.
The estimated five-year survival after PTE is 85 to 90 percent, compared with the estimated 50 percent five-year survival post-lung transplantation. Accordingly, performing PTE significantly prolonged the estimated life expectancy of this young woman.
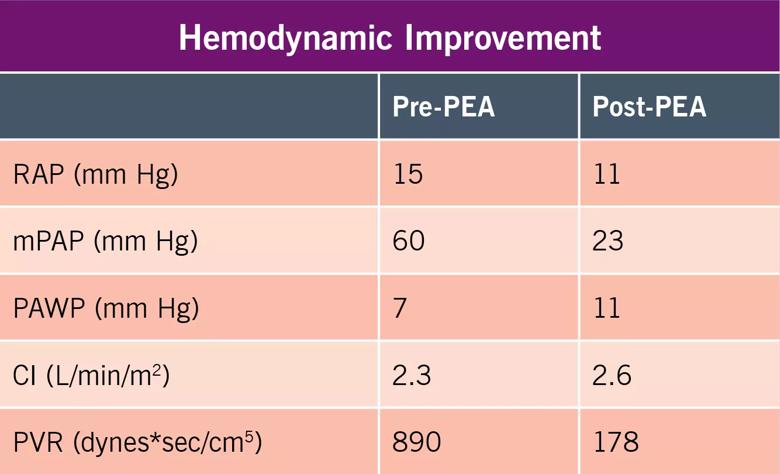
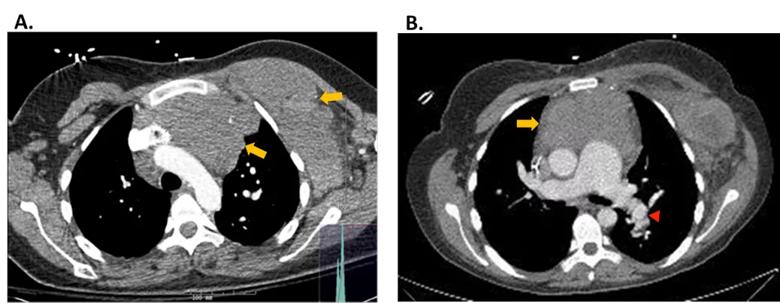
Figure 1. CT Chest
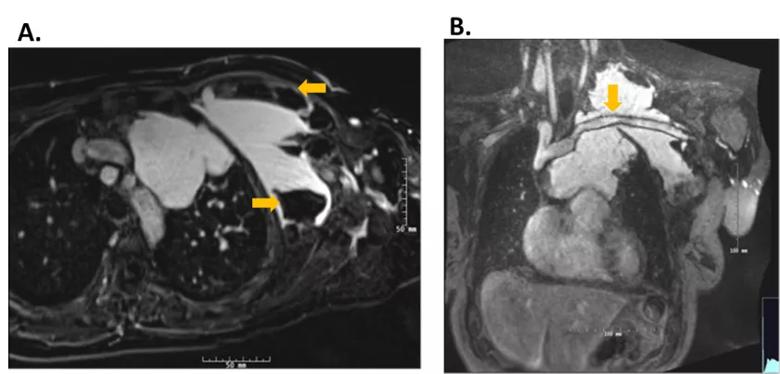
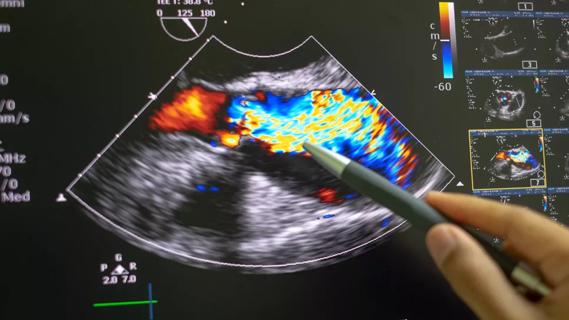
Figure 2. Magnetic resonance angiography.
Dr. Heresi, Medical Director of the Pulmonary Thromboendarterectomy Program in the Respiratory Institute, can be reached at 216.636.5327 or heresig@ccf.org. Dr. Gomes, a vascular medicine specialist, can be reached at 216.444.3352 or gomesm2@ccf.org. Dr. Karuppasamy, an interventional radiologist, can be reached at 216.444.0412 or karuppk@ccf.org. Dr. Levitin, an interventional radiologist, can be reached at 216.444.2244 or levitia@ccf.org. Dr. Smedira, a cardiothoracic surgeon, can be reached at 216.445.7052 or smedirn@ccf.org.
Advertisement
Advertisement

Volatile organic compounds have potential in heart failure diagnostics

Caregivers are provided with real-time bronchoscopy patient findings
Insights for diagnosing, assessing and treating
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients

New program sets out to better support underserved patient populations
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality

Lessons learned from cohorting patients and standardizing care
New tools and protocols to improve care