Each unprevented infection brings large clinical and economic burdens
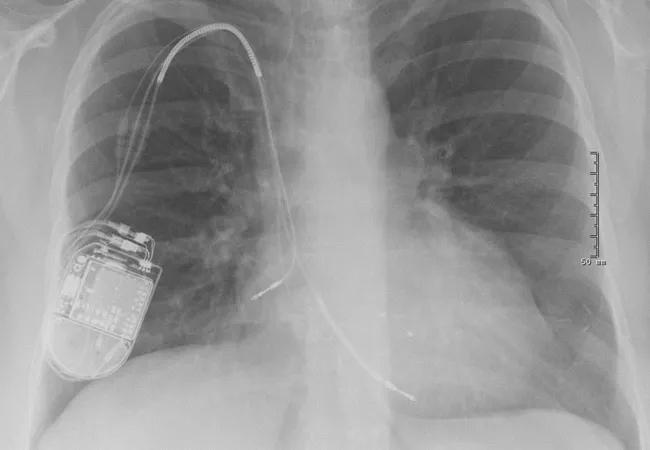
Infections following changes, upgrades or revisions to cardiac implantable electronic devices (CIEDs) have enormous clinical and financial impacts on patients, hospitals and the healthcare system, a new analysis of the Cleveland Clinic-led WRAP-IT trial has found.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The analysis reveals a multitude of negative effects of CIED infection: a threefold rise in 12-month mortality, therapy interruption lasting from days to more than a year, multiple additional clinic visits and hospitalizations, months-long diminishment in patient quality of life, and thousands of dollars in losses for hospitals for each infection.
“CIED infection is a major event,” says Cleveland Clinic electrophysiologist Bruce Wilkoff, MD, lead author of the analysis and steering committee chair for the WRAP-IT trial. “The data we’ve gathered corroborate and extend understanding of the real-world impact of CIED infection. They should create awareness of the need for systemwide efforts for infection prevention.”
Dr. Wilkoff and colleagues presented the analysis at the American Heart Association 2019 Scientific Sessions on November 17. It marks the first prespecified analysis conducted on the clinical and economic impact of CIED infection. Previous data on the issue have been inferred or retrospectively collected.
The current study was planned as an as-treated analysis of the international WRAP-IT trial, a randomized, prospective, single-blind, multicenter investigation of the impact of an absorbable, antibiotic-eluting envelope on reducing CIED-related infections. Nearly 7,000 patients who were undergoing a CIED procedure — de novo device implantation, generator replacement, system upgrade, or pocket or lead revision — were randomly assigned to receive the envelope or not. All patients received standard-of-care infection prevention measures.
Advertisement
Initial results of WRAP-IT were published in the New England Journal of Medicine earlier this year and showed a 40% reduction in major CIED infections within 12 months of the CIED procedure among patients receiving the envelope. Across the entire cohort, 75 major CIED infections occurred in 67 patients in the first 12 months of follow-up. Infections were defined as major if they resulted in CIED extraction or revision, long-term antibiotic treatment with infection recurrence, or death.
The current analysis examined a number of clinical outcomes among these WRAP-IT patients with major CIED infection: mortality, quality of life, interruption of CIED therapy, need for hospitalization, and hospital and clinic days.
“We had the impression that CIED infection was a major catastrophe, and we wanted to evaluate its magnitude from every angle,” Dr. Wilkoff explains.
The investigators found major CIED infection to be associated with the following:
Advertisement
The analysis also assessed the economic impact of major CIED infection. Payer costs were assigned using Medicare national payment data, and hospital and patient costs were determined from comparable hospital admissions in a separate administrative database. All costs are in 2017 U.S. dollars.
The mean cost of CIED infection treatment was $55,547 for the treating hospital, with a mean Medicare fee-for-service cost of $26,867. For Medicare fee-for-service patients, the mean out-of-pocket expense for an infection-related hospitalization was $2,156.
“Everyone lost — patients, Medicare, hospitals,” Dr. Wilkoff notes. “The mean hospital margin for Medicare fee-for-service patients was a loss of about $30,000 per infection.”
“While WRAP-IT showed that the antibiotic envelope significantly reduces infections, that is only one aspect of infection prevention,” Dr. Wilkoff concludes. “We need to be focusing on implantation technique, perioperative antibiotic therapy and other aspects of the system to reduce infection rates.”
“Studies of the cost-effectiveness of using the antibiotic-eluting envelope are forthcoming,” notes Oussama Wazni, MD, Section Head of Cardiac Electrophysiology and Pacing at Cleveland Clinic.
“From a patient’s perspective, CIED infection is not a one-time risk but rather a lifetime risk that is especially relevant every time a patient undergoes device replacement for battery depletion or other reasons,” adds Cleveland Clinic electrophysiologist Khaldoun Tarakji, MD, MPH, global principal investigator of WRAP-IT. “This analysis is another reminder that despite all the proper therapy for CIED infection with system removal and antibiotic treatment, the morbidity and mortality remain high. That’s why prevention is key, and it represents a shared responsibility among clinicians, healthcare systems and device manufacturers.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable