Matched cohort study finds marked survival disadvantage with radiation
Among patients undergoing surgical aortic valve replacement (SAVR) for severe aortic stenosis, long-term survival is significantly worse in the subpopulation whose aortic stenosis is due to chest radiotherapy (XRT). So finds one of the largest-ever investigations to compare long-term survival following SAVR between patients with XRT-associated severe aortic stenosis and a matched population from the same time frame whose severe aortic stenosis is not related to XRT.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Valvular heart disease develops in as many as 8 in 10 patients with previous mediastinal radiotherapy, and the aortic and mitral valves are most often affected,” says study co-author Brian Griffin, MD, Section Head of Cardiovascular Imaging at Cleveland Clinic. “A recent study from our institution found significantly elevated long-term mortality among patients with prior chest radiation who underwent open-heart surgery. In this new study we assessed how prior radiation affected long-term survival specifically in patients undergoing SAVR and to identify predictors of mortality in this setting.”
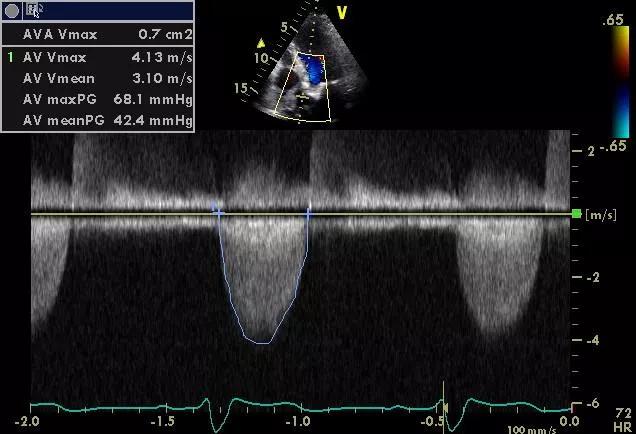
The new study, published in the Journal of the American Heart Association, was an observational cohort analysis of patients with severe symptomatic aortic stenosis who underwent SAVR at Cleveland Clinic from 2000 to 2015. Within this population, 172 patients were identified who had undergone mediastinal irradiation before developing aortic stenosis. This “XRT group” was matched 1:1 on the basis of age, sex, type and timing of SAVR, and aortic valve area with 172 SAVR patients with no history of mediastinal irradiation (comparison group).
At 5.7 ± 3 years of post-SAVR follow-up, mortality was significantly higher in the XRT group (28 percent) than in the comparison group (7 percent) (P < .001). Nearly all deaths in the XRT group were due to cardiorespiratory disease or multiorgan failure (not recurrent malignancies).
The significant increase in mortality risk conferred by XRT was observed across all patient subgroups analyzed, including those based on age, sex, presence/absence of obstructive coronary artery disease (CAD), Society of Thoracic Surgeons (STS) score, type of surgery (AVR alone vs. AVR plus CABG vs. AVR plus aorta) and others.
Advertisement
Multivariable survival analysis of the total study cohort showed only two factors to be independently associated with elevated long-term mortality:
Notably, while long-term survival was dramatically worse in the XRT group, there was no large difference in short-term survival.
“Although our data on the cause of death after SAVR in the radiation group are limited, it appears that cardiopulmonary disease was a common mechanism,” says the study’s corresponding author, Cleveland Clinic cardiologist Milind Desai, MD. He explains that this may be attributable to the likelihood that prior mediastinal XRT introduces numerous technical problems at the time of SAVR due to radiation-induced fibrosis of neighboring tissues, adhesions and presence of multiple cardiac lesions.
The authors note that while their retrospective, single-center findings require further validation, these results raise the question of alternatives to SAVR, including transcatheter aortic valve replacement (TAVR), for managing XRT-associated severe aortic stenosis.
“Robust data on long-term outcomes in patients with heart disease after radiation who have undergone TAVR are presently lacking,” observes Dr. Desai. “And we cannot assume that percutaneous approaches to radiation-associated heart disease are necessarily superior. For instance, last year our group published a paper demonstrating that patients with obstructive CAD due to prior radiation therapy who underwent percutaneous coronary intervention (PCI) had higher mortality than did a matched control PCI population. So careful investigation of TAVR for patients with radiation-associated aortic stenosis is needed.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable