How and why MRI’s role in fetal neuroimaging has expanded
By Unni Udayasankar, MD, FRCR
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Early and accurate diagnosis of fetal anomalies can inform decision making on patient management, fetal surgery, possible transfer to a specialized center, and mode of delivery. Although prenatal ultrasound remains the primary modality for evaluating abnormalities in a developing fetus, the role of fetal MRI in prenatal diagnosis continues to expand — specifically in challenging clinical situations.
MRI can be particularly useful for fetal neuroimaging in the following settings:
Cleveland Clinic’s Imaging Institute works closely with our maternal-fetal medicine (MFM) specialists to provide ultrafast fetal MRI studies. For pregnancies complicated by serious maternal or fetal conditions, Cleveland Clinic opened a unique Special Delivery Unit (SDU) in 2012 to provide comprehensive care in the perinatal period for the newborn and/or mother. Our team comprises pediatric radiologists, MFM specialists and neonatal neurologists.
The American College of Radiology recommends that fetal MRI be performed only after 20 weeks of gestational age. Before this age, MRI is unlikely to add significant incremental information in view of the small size of the fetus. Additionally, the effect of MR energy deposition in early fetuses is incompletely understood.
A 1.5-tesla (1.5T) MRI system is routinely used for fetal MRI. Although some centers are using 3T systems, specific absorption rate, a measure of energy deposition from the system, should be measured and maintained within the recommended levels. Higher-resolution surface MRI coils are used, with the patient best imaged supine or in the left lateral decubitus position. Sedation is not routinely performed.
Advertisement
There are currently no fetal indications for contrast administration. Interpretation of MRIs is often performed in correlation with images from prenatal ultrasound.
The principal theoretical risk of fetal MRI relates to excess tissue heating, which has been associated with growth retardation and congenital malformations in various animal models.
Current American College of Radiology recommendations regarding the safety of fetal MRI emphasize that no studies have conclusively documented or reproducibly demonstrated harmful effects to the pregnant woman or the fetus.
The most common neuroimaging indications for fetal MRI at Cleveland Clinic are:
Ventriculomegaly is one of the most common indications for fetal MRI. Lateral ventricular measurement at the level of atria exceeding 10 mm constitutes ventriculomegaly. The etiology of fetal ventriculomegaly includes atrophic/destructive processes (Figure 1), dysgenetic abnormalities and obstructive hydrocephalus (Figure 2). MRI provides further details of ventricular configuration and contour and can point to underlying parenchymal anomalies. Changes of infection, ischemia and hemorrhage also can be readily identified on fetal MRI (Figure 3).
Other anomalies of cortical maturation, including agenesis of the corpus callosum, lissencephaly, polymicrogyria, pachygyria and schizencephaly, are also better appreciated on MRI than on ultrasound.
MRI is often performed when agenesis of the corpus callosum (ACC) is suspected on ultrasound. ACC can be complete or partial. Parallel orientation of lateral ventricles, colpocephaly, absence of septum pellucidum, high-riding third ventricle, interhemispheric cysts, and a classic moose horn pattern of frontal horns on coronal images are a few diagnostic features of ACC (Figure 4). Associated structural anomalies of the brain also can be ruled out on MRI.
Advertisement
Posterior fossa cysts and cystlike malformations are often encountered in fetal neuroimaging with MRI. These range from incidental retrocerebellar cysts, arachnoid cysts and mega cisterna magna to the Dandy-Walker continuum that includes classic Dandy-Walker malformation, Dandy-Walker variant (Figure 5) and Blake’s pouch cyst. Diseases in the Dandy-Walker spectrum are often associated with other developmental anomalies as well as ventriculomegaly. When prenatal ultrasound is indefinite, MRI helps to elucidate anatomic details of the posterior fossa and improve diagnostic clarity.
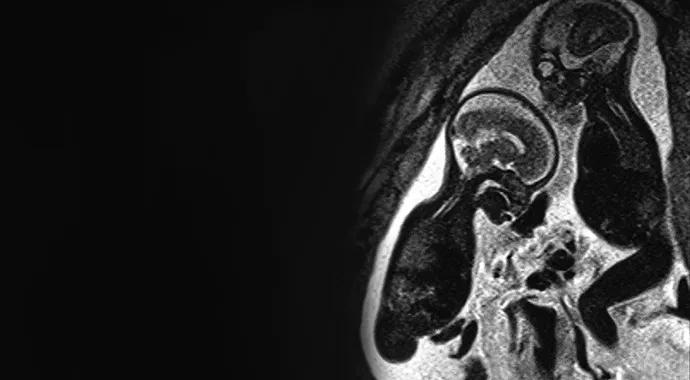
Spinal dysraphism is part of a heterogeneous group of congenital disorders of the spine otherwise known as neural tube defects. Open spinal dysraphism or myelomeningocele (Figure 6) is one of the most severe congenital disorders of the CNS, with varying degrees of mental retardation, bowel and bladder dysfunction, and severe motor disabilities. Fetuses with higher (thoracolumbar) defects are associated with severe functional limitation, with progressive improvement seen with more caudal lesions.
The cerebrospinal fluid (CSF) leak through the myelomeningocele is shown to be the underlying cause for hindbrain herniation, features of type II Chiari malformation and hydrocephalus in these patients. With recent advances in fetal surgery, it is now possible to perform in utero repair of open spinal dysraphisms in selected patients. A recent multicenter randomized prospective trial showed that fetal surgery results in better clinical outcomes compared with postnatal repairs — specifically, a significant reduction in the need for ventriculoperitoneal shunt placement along with substantial improvement in overall neuromotor function and reversal of hindbrain herniation.
Advertisement
Fetal MRI, along with prenatal ultrasound, plays a key role in identifying spinal dysraphism and guiding therapy. Prenatal ultrasound has a high sensitivity in detecting spinal defects. Fetal MRI helps to further characterize spinal abnormalities, including lesion level, presence or absence of a covering membrane, and size of the bony defect. MFM specialists, neonatal neurologists, fetal surgeons and neurosurgeons use MRI findings to assess eligibility for fetal surgery. Recent studies show the potential of fetal MRI in predicting neonatal outcomes in myelomeningocele.
Closed neural tube defects (which usually include meningocele, lipomeningocele, terminal myelocystocele and split cord malformation) are not usually associated with severe functional limitation or structural abnormalities of the CNS. Occasionally, closed neural tube defects may be mistaken for more severe open defects. Fetal MRI could aid in diagnosis by identifying the intact covering over the defect.
Fetal MRI has emerged as a robust supplement to ultrasound in the diagnosis of fetal abnormalities. Technical advances and widespread availability continue to expand the role of MRI in fetal neuroimaging, specifically in cases with incomplete or complex sonographic findings.

Figure 1. Hydranencephaly. Coronal HASTE T2 sequence shows near-total loss of the supratentorial brain parenchyma, which is replaced by a large space containing cerebrospinal fluid (arrows). Posterior fossa structures are normal.
Figure 2. Severe hydrocephalus due to aqueductal stenosis. Coronal HASTE T2 sequence shows massively dilated lateral ventricles (arrows) with focal discontinuity of the right lateral ventricle (white arrow), compatible with ventricular rupture.
Advertisement
Figure 3. Germinal matrix hemorrhage. Axial HASTE T2 image shows irregular hypointense signal in the left germinal matrix region (arrows).
Figure 4. Agenesis of the corpus callosum. Axial HASTE T2 image shows absence of the corpus callosum with parallel orientation of the lateral ventricles. The occipital horns are dilated (arrows) when compared with the frontal horns (colpocephaly).
Figure 5. Dandy-Walker variant. Sagittal HASTE T2 image shows absence of the inferior vermis and a posterior fossa cyst (arrows) that communicates with the fourth ventricle.
Figure 6. Lumbosacral myelomeningocele with type II Chiari malformation. Sagittal HASTE T2 image shows an open neural tube defect (myelomeningocele) extending from the midlumbar level down to involve the entire sacral region (arrows). Note small posterior fossa and low-lying cerebellar tonsils. Polyhydramnios and rocker bottom foot are also noted (open arrow).
Dr. Udayasankar is a pediatric radiologist in Cleveland Clinic’s Imaging Institute who focuses on pediatric neuroradiology. He is also Assistant Professor of Radiology at Cleveland Clinic Lerner College of Medicine.
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade