OCT Angiography critical in recent case
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A young, pregnant woman presented for evaluation of a new scotoma associated with other mild systemic symptoms, including an episode of presyncope after the scotoma appeared. It was unclear whether her systemic symptoms were related to her visual disorder.
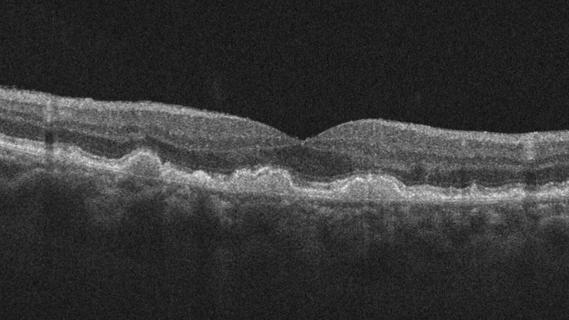
Her visual acuity was excellent in both eyes. Ophthalmic examination was unremarkable. In this case, the differential diagnosis included retinal disorders, such as focal ischemia or vascular occlusive disease, and optic nerve disorders, such as optic neuropathy. Diagnostic testing with spectral domain optical coherence tomography (OCT) was performed and identified a focal area of increased reflectivity in the inner nuclear layer, suggestive of paracentral acute middle maculopathy (PAMM).
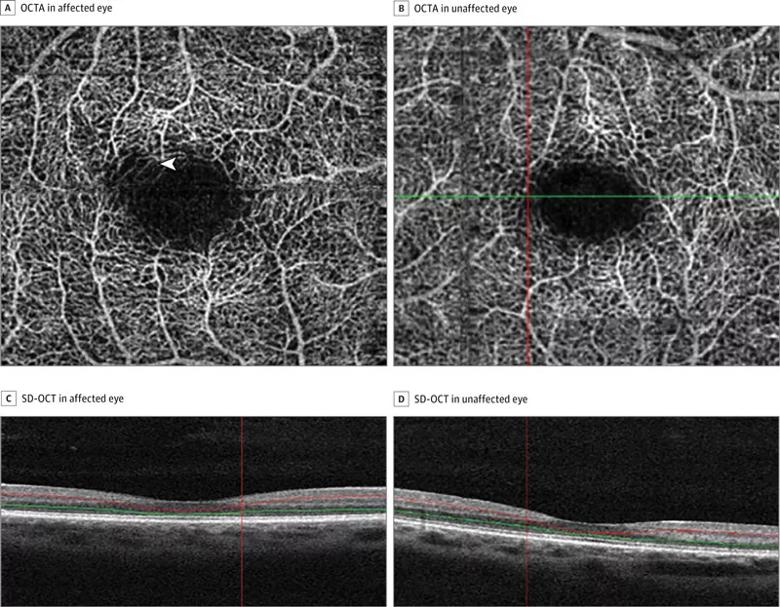
Figure 1: Near-Infrared Reflectance (NIR) Imaging and Spectral-Domain OCT (SD-OCT) of a PAMM lesion in the Right Eye. Initial presentation A, B. NIR imaging shows dark lesion (arrow in B) in superotemporal macula. C. SD-OCT indicates corresponding focal hyperreflectivity (arrowhead) (N = nasal; S = superior; T = temporal). One month later D, E. NIR imaging shows resolution of lesion F. SD-OCT of corresponding inner nuclear layer thinning (arrow).
PAMM is thought to occur due to focal ischemia in the deep retinal vascular capillary bed. Multiple conditions may result in PAMM or Pamm-like lesions including artery occlusions, inflammatory conditions, and vein occlusions. Often this subtle finding is only apparent on imaging and cannot be visualized on clinical exam.
Advertisement
In cases of suspected retinal vascular abnormalities, fluorescein angiography is often performed. In this case, given patient’s pregnancy, fluorescein angiography was not an ideal option.
We turned instead to OCT angiography (OCTA). In 2015, OCTA was a new and emerging technology. OCTA provides high resolution, 3D visualization of retinal vascular flow, in effect providing flow maps for specific areas of the retina. One of the advantages of OCTA in this case was the ability to visualize vascular flow without intravenous dye injections.
Utilizing OCTA, we were able to see a flow void in the area that corresponded with the patient’s scotoma and the abnormality seen on OCT. OCTA confirmed the vascular nature of her condition and helped support the diagnosis of PAMM. The patient remained stable without any progression of her condition.
To read the full case, see its recent presentation in JAMA Ophthalmology.
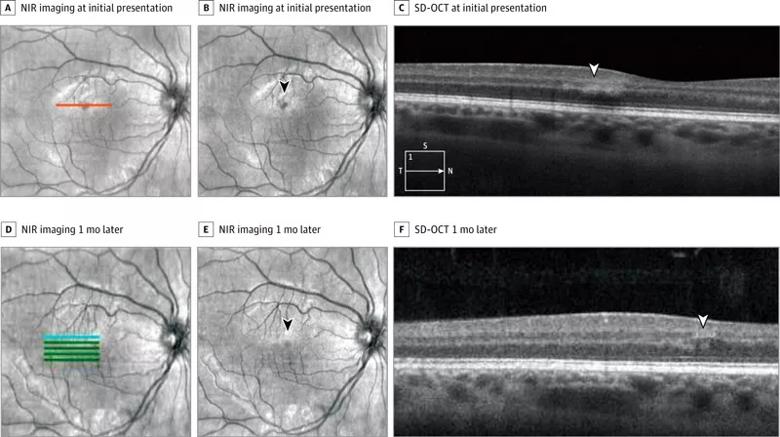
Figure 2: OCTA and SD-OCT 2 months after initial presentation A. OCTA shows outer retinal capillary nonperfusion (arrow) at lesion in right eye B. OCTA of intact outer retinal capillary perfusion in left eye. C, D. Corresponding SD-OCT shows OCTA segmentation (between red and green lines).
In the last year, the FDA has cleared two OCTA systems for ophthalmic use. At Cole Eye Institute, we are actively engaged in clinical studies examining the role of OCTA in retinal disease. We have enrolled over 300 patients in three trials in the last year.
OCTA is noninvasive and very efficient, typically requiring less than a few minutes for image acquisition. Although this technology is quite exciting, significant challenges still exist. Current OCTA systems have a limited field-of-view (e.g., 3×3 mm, 6×6 mm), whereas ultra-widefield FA allows imaging of nearly the entire retina.
Advertisement
OCTA also provides outstanding information related to active flow and flow voids. However, with current technology, visualization of leakage is not yet possible.
OCTA is one of the hottest areas of interest and research in ophthalmology. It is an exciting and emerging technology that may have significant advantages in imaging select cases. Many questions remain: For which conditions does it really make a difference? How does OCTA change clinical management? Does it improve outcomes?
Ongoing clinical studies will help answer some of these important questions.
Dr. Ehlers is the Norman C. and Donna L. Harbert Endowed Chair for Ophthalmic Research, Vitreoretinal Service, Cole Eye Institute
Advertisement
Advertisement
Early data shows risk is 73% higher in patients with lupus, 40% higher in patients with rheumatoid arthritis

Identifies weak spots in the cornea before shape change occurs

Study highlights the value of quantitative ultra-widefield angiography

Switching medications may decrease treatment burden and macular fluid

Interventions abound for active and stable phases of TED

Corneal imaging and interpretation play a major role

Cole Eye Institute imaging specialists are equal parts technician, artist and diagnostician

Effect of low-dose atropine and dual-focus contact lenses is unknown in patients with comorbid eye conditions