Sampling of outcomes and volumes of note
When a center has a vascular surgery case volume exceeding 7,500 a year and one of the oldest and largest vascular medicine programs in the U.S., it’s bound to yield some noteworthy volume and outcome stats. This infographic shares a sampling of them.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
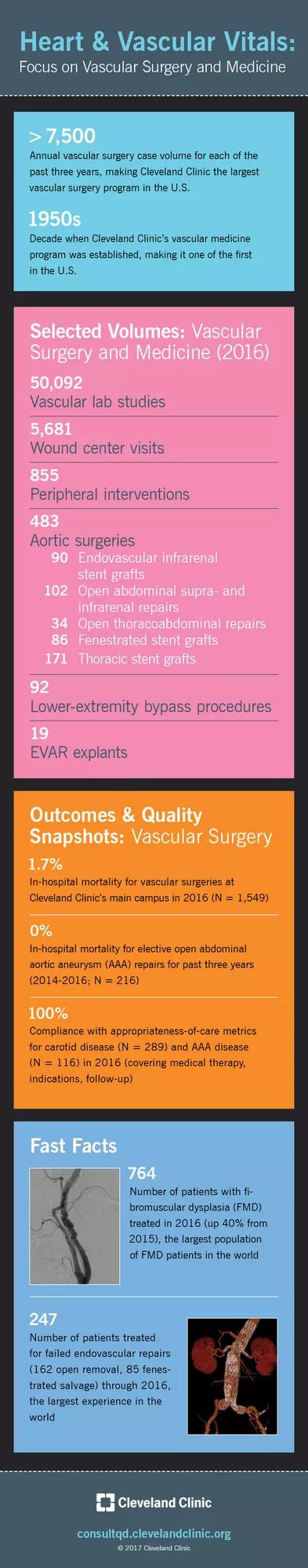
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c9b996ee-cfca-44dd-afa0-9fdc2dd9899e/17-HRT-3383-Vitals-Infographic-CQD-FNL_jpg)
The annual vascular surgery case volume for each of the past three years is greater than 7,500, making Cleveland Clinic the largest vascular surgery program in the U.S. The program was established in the 1950s, making it one of the first in the U.S. In 2016, over 50,000 vascular lab studies were performed at Cleveland Clinic. The wound center saw almost 6,000 patients, and the interventional team performed almost 1,000 peripheral interventions. The surgical team performed 483 aortic surgeries, including 90 endovascular infrarenal stent grafts, 102 open abdominal supra- and infrarenal repairs, 34 open thoracoabdominal repairs, 86 fenestrated stent grafts and 171 thoracic stent grafts. The surgical team also performed 92 lower-extremity bypass procedures and 19 EVAR explants.
The in-hospital mortality for vascular surgeries at Cleveland Clinic’s main campus in 2016 was 1.7 percent (N = 1,549). For elective open abdominal aortic aneurysm (AAA) repairs, the in-hospital mortality rate was 0 percent from 2014 to 2016 (N = 216). In addition, the team accomplished 100 percent compliance with appropriateness-of-care metrics for carotid disease (N = 289) and AAA disease (N = 116) in 2016 (covering medical therapy, indications and follow-up.
In 2016, the team saw 764 patients with fibromuscular dysplasia (FMD), 40 percent more patients than in 2015 and the largest population of FMD patients in the world. They treated 247 patients for failed endovascular repairs (162 open removal, 85 fenestrated salvage) through 2016, the largest experience in the world.
Advertisement
Advertisement
A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy
Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable