Early detection can improve treatment, quality of life

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In 1970, Alvan R. Feinstein, MD, defined comorbidities as a greater than coincidental association of two conditions in the same individual. The term does not imply direction or causation; the disorders might co-occur by chance or may share genetic, environmental or other mechanisms.
At Cleveland Clinic’s Neurological Institute, an innovative database known as the Knowledge Program© allows treating physicians to identify depression and other neuropsychiatric comorbidities in children with epilepsy and to track major epilepsy outcomes. Future directions include the tailoring of the program to identify comorbidities that are present in preschoolers with epilepsy.
Children with epilepsy are affected by neurocognitive, psychiatric, medical and social comorbidities. The association of epilepsy with learning disabilities, cognitive problems, low IQ and cerebral palsy has been well recognized for many years. Therefore, screening for and diagnosis of these conditions in children with epilepsy have been early and very consistent.
Now, clinicians are recognizing a growing need to screen for other important neuropsychiatric comorbidities that sometimes have been neglected despite the obvious association with epilepsy. Cleveland Clinic’s Knowledge Program is an example of an innovative, high-tech tool that can facilitate this type of monitoring.
What follows are some common questions about screening children with epilepsy for neuropsychiatric comorbidities.
Why screen for neuropsychiatric comorbidities? There is a bidirectional relationship between epilepsy and neuropsychiatric comorbidities. The existence of comorbidities affects our selection of anti-epileptic treatment. Also, the effects of anti-epileptic medication can cause, or worsen, some comorbidities.
Advertisement
Children with epilepsy often have unmet needs for medical and mental health along with poor coordination of care. Therefore, screening and early identification of these comorbidities can lead to more comprehensive care delivery.
Which children are at greatest risk for neuropsychiatric comorbidities? Certain biological, social and treatment-relatedfactors increase the risk for comorbidities in childrenwith epilepsy:
• Biological factors ‒ younger age at seizure onset, history of cognitive impairment, temporal or frontal lobe epilepsies and refractory seizures
• Social factors ‒ lower socioeconomic status, lower parental education level and poorer family function
• Treatment-related factors ‒ longer period of treatment with anti-epileptic medications and polytherapy
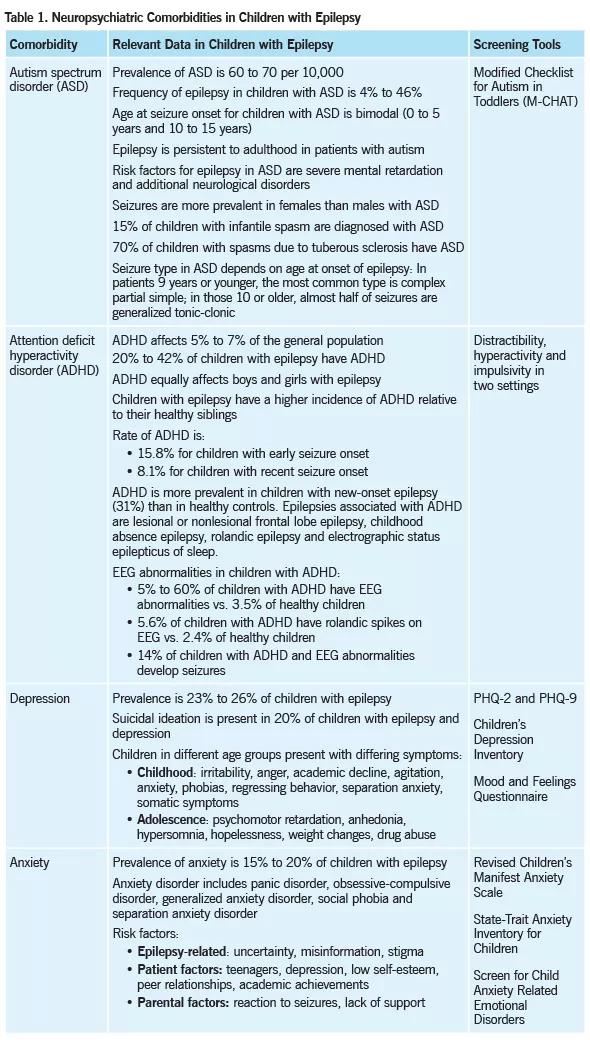
Which neuropsychiatric comorbidities should be screened for in children with epilepsy? A number of neuropsychiatriccomorbidities can be found in children with epilepsy, includingautism spectrum disorder (ASD), attention deficit hyperactivitydisorder (ADHD), depression and anxiety. Information relevant tothese conditions in children with epilepsy is found in Table 1.
The age at onset of these comorbidities in children can vary, so any screening program needs to take this variable into account.
ASD. Initial ASD symptoms are present in the toddler years. The diagnosis of ASD often is not made until age 2 or 3 years, after the symptoms are recognized. The average age at diagnosis of ASD is about 6 years. Screening for ASD needs to target toddlers and preschoolers.
Advertisement
ADHD is the most common disorder in preschool- and school-age children with epilepsy. According to the DSM-IV, the diagnosis of ADHD is made when there are six out of nine behavioral and functional symptoms of inattention, hyperactivity and impulsivity, with onset before age 7 years and more than six months’ duration of symptoms. There is a variety of options to treat ADHD today.
Depression and anxiety affect at least one-third of school-age children and teenagers with epilepsy. There are well-established standardized screening tests for depression and anxiety in children (see Table 1). The selection of one screening tool over another depends on the time frame available for the screening and validation characteristics of the tool.
One cannot overstate the importance of a multidisciplinary team in the identification, diagnosis and management of neuropsychiatric comorbidities in children with epilepsy. Multidisciplinary teams vary, but ideally they should include specialized nurse practitioners and clinical nurses, pediatricians, behavioral specialists, pediatric neurologists and epileptologists, and child psychiatrists.
At Cleveland Clinic, children with epilepsy and their families receive diagnosis and management not only from our pediatric epilepsy specialists, but also from epilepsy specialized social workers, medical ethicists, clinical nurses, nurse practitioners, child psychologists and child psychiatrists. A vast network of physicians facilitates easy referral to pediatricians and behavioral pediatricians at our main campus and community sites within the region.
Advertisement
Dr. Pestana Knight is a staff physician in the Pediatric Epilepsy Section of the Epilepsy Center in Cleveland Clinic’s Neurological Institute. Her clinical and research interests include pediatric epilepsy outcomes, including quality of life, early detection and treatment of pediatric comorbidities in children with epilepsy, management of epileptic encephalopathy, and electroencephalography.
-Feinstein A. The pre-therapeutic classification of co-morbidity in chronic disease. J Chron Dis. 1970;23:455-468.
–Canitano R. Epilepsy in autism spectrum disorders. Eur Child AdolescPsychiatry. 2007;16(1):61-66.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade