Incidence may be higher than previously believed

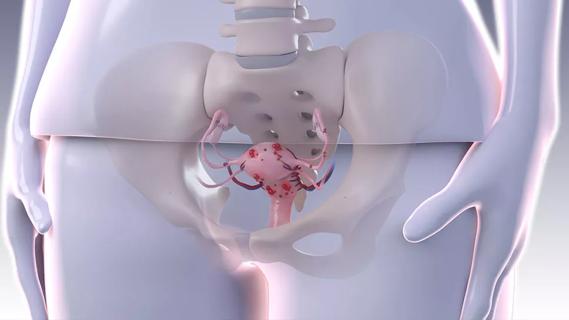
Extrapelvic deep endometriosis may be more common than previously believed, according to the results of a recent systematic review of the literature.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Without comparative studies, we don’t have recommendations about how best to diagnose and treat extrapelvic endometriosis. Clinical suspicion tends to be low, and in general, physicians may not know what to look for,” states Rosanne M. Kho, MD, a gynecologist with the Cleveland Clinic’s Ob/Gyn & Women’s Health Institute and associate editor of the Journal of Minimally Invasive Gynecology. “As a result, the diagnosis and management of extrapelvic endometriosis at distant sites can be quite challenging.”
Endometriosis is thought to develop as part of retrograde menstruation, when endometriotic cells reach the abdominopelvic region via the fallopian tube, undergo neoangiogenesis and implant at potentially distant sites. The condition is labeled deep endometriosis if these endometriotic nodules are more than 5 mm in size.
“Primary extrapelvic endometriosis can affect nearly every organ system in the body. We once thought it was rare, but our review indicates that the incidence may be higher than originally believed,” Dr. Kho notes.
In the review, researchers identified more than 5,000 articles related to extrapelvic endometriosis. After excluding duplicates, review articles and those involving the bowel, cancer or scar endometriosis, 179 were included in the final analysis. For the purposes of this review, data was organized by site of extrapelvic endometriosis.
Abdominal endometriosis was separated into two categories: parietal endometriosis (PE), which included primary lesions in the abdominal wall, groin and perineum; and visceral endometriosis (VE), which included lesions in the abdominal organs.
Advertisement
For PE, the mean age at clinical presentation was 38.5 years (range, 25-73). Common presenting symptoms were a palpable mass, parietal pain and umbilical bleeding. Diagnosis generally involved ultrasound, magnetic resonance imaging or computed tomography. Surgery — generally wide local excision — was performed in 97% of the PE cases. General surgeons performed 71.1% of these procedures, with only 15.7% performed by a gynecologist. Adjuvant hormonal treatment was rarely reported.
For VE, the mean age at presentation was 40.3 years (range, 25-73). Patients with liver endometriosis presented with upper abdominal pain and abdominal mass; patients with kidney endometriosis reported flank pain, hematuria and pyelonephritis; patients with pancreatic endometriosis reported epigastric pain; and patients with liver endometriosis presented with acute liver failure and upper abdominal pain. CT was commonly used in the diagnosis of VE, and most patients were treated with surgery. All patients reported symptom improvement.
Lesions involving the diaphragm, pleura and lung were grouped as thoracic endometriosis (TE). At clinical presentation, the mean age of patients was 22.6 (range, 16-54). The most common symptom was pneumothorax. Lesions were generally found through chest X-ray or CT, and confirmed by histologic or immunohistochemical analysis. In most cases, lesions associated with TE were removed surgically, and adjuvant hormonal therapy was reported in only 15.5% of cases.
Other, rarer sites of endometriosis were grouped together, and included lesions involving the vascular, lymphatic and central nervous systems, the brain, skeletal muscles and peripheral nerves. Common presenting symptoms included paresthesia and cyclic pain with radiation according to topographic site involvement, and dysmenorrhea. At clinical presentation, patients ranged in age from 21 to 58 years. MRI was used for preoperative evaluation, showing a hyperintense T1 or isointense T2 lesion. Surgical excision with adjuvant hormonal therapy was used in many cases; however, one patient with brain endometriosis was treated with gonadotropin-releasing hormone agonist (GnRHa) and bilateral salpingo-oophorectomy, and one patient with nasal endometriosis was treated with GnRHa alone.
Advertisement
“Extrapelvic endometriosis may not be as rare as we originally thought, and clinical presentation varies widely,” Dr. Kho says. “With limited evidence, we can’t determine the best treatment choice for each type and extent of extrapelvic endometriosis. Detailed case reporting and validated patient assessment tools — perhaps through a worldwide patient registry — would go a long way toward developing consistent standards of care for patients with this debilitating condition.”
Advertisement
Advertisement
Counseling and careful surgical considerations are key

Deprivation is linked to impaired glucose intolerance and racial disparities

Perioperative prophylaxis and class III obesity

Artesunate ointment is safe well and tolerated patients with vulvar intraepithelial neoplasia

Endoscopic balloon dilation during pregnancy helps optimize outcomes

Researchers examine waste and implore colleagues to take action

Mode of delivery does not affect patient satisfaction