Researchers share their innovative approach
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/cd3626f2-8b87-4370-a8bc-43cfec2138e4/19-ORT-1460-PJI-CQD-Hero_jpg)
19-ORT-1460-PJI-CQD-Hero
By Anabelle Visperas, PhD; Nicolas Piuzzi, MD; Alison Klika, MS; Anna C.S Samia, PhD; Wael Barsoum, MD; and Carlos Higuera-Rueda, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Periprosthetic joint infection (PJI) is a catastrophic complication of total joint arthroplasty,1–3 which accounts for 18%-30% of revision hip4,5 and 19% of revision knee6 replacements in the United States. Projections have estimated it will cost over $1.6 billion with a caseload of 70,000 revisions per year by 2020.7 The five-year mortality rate is close to 26%, which is as high as that
for many common cancers.8 While treatment options, including a combination of irrigation and debridement (I&D), intravenous antibiotics, and one- and two-stage revisions, are commonly utilized, failure rates are still high at around 30% to 50%. This is mainly related to the formation of bacterial biofilms and the reduced capabilities of antibiotics to have a significant effect on
them. Thus, there is a dire need to improve treatment options and create innovative alternatives.
Both diagnosis and treatment are difficult due to the impenetrable biofilm produced by many bacterial species responsible for PJI.9,10 This biofilm decreases the metabolism of bacteria and protects it from antibiotic therapies and the immune system. Therefore, both diagnosis and treatment strategies can benefit from disrupting biofilm formation. Bacterial biofilm has become a hot topic in recent years in the microbiology field, where novel treatment strategies are being developed. Nevertheless, an animal model that is clinically representative of human PJI needs to be developed to test these treatment modalities.
Many groups have begun developing various PJI animal models, utilizing rodents (mice and rats), rabbits, dogs and goats. Each animal model has its own set of advantages and disadvantages.11 While rodents are relatively cheap and are appealing for high-throughput testing, their joint space volume, bone physiology and size can be a hindrance. Larger animals have several advantages.
They are able to handle multiple surgeries, as is commonly the case in PJI treatment in humans; relative to rodents, they have musculoskeletal and immunological systems similar to human ones; and larger animals have sufficient joint space volume for potential future treatment applications. However, their exorbitant costs compared with that of rodents and the ethical concerns
associated with large animal research need to be considered.
Advertisement
Carli et al.12 suggested four standardized criteria that future models need to include to be clinically representative of PJI:
1. The animal must have musculoskeletal and immunological properties similar to those of humans.
2. The implant should be made of relevant material, bear weight and reproduce the periprosthetic environment.
3. The study should use clinically relevant bacteria that can reliably produce biofilm on implant.
4. The study should should employ a methodology to measure biofilm, bacterial burden and immunological response.
Our group has built on existing models and the recommendations of peers to develop a clinically relevant rabbit model of knee PJI (Figure 1). We used rabbits as our model of choice due to their size, joint space volume, hardiness to multiple surgeries and musculoskeletal similarities to humans (criterion 1). This rabbit model utilizes a custom-made titanium tibial press-fit implant that allows for immediate weight-bearing after surgery and full use of the limb within seven days of surgery (criterion 2).
This implant has an articular surface that interacts with the periprosthetic joint space and a shaft that interacts with the intramedullary space, similar to implants used in humans (Figure 2A). It also uses a clinically relevant bacterial strain, Staphylococcus aureus, which accounts for up to 38% of knee and hip PJIs.3 It is bioluminescently marked for easy tracking and identification (criterion 3).
We have developed multiple readouts for productive infection and bacterial burden, including scanning electron microscopy of the implant to assess biofilm formation (Figure 2B) and cultures/bioluminescence to assess bacterial burden (Figure 2C). Peripheral white blood cell and C-reactive protein levels are also being assessed using this model and may be further expanded to include synovial fluid sampling for cellular analysis (criterion 4). We have built on current models and gone beyond the recommendations of Carli et al. by adding an I&D step two weeks after implantation and inoculation, which is clinically relevant and has not been done with any other PJI animal model to date. This rabbit model of knee PJI enables the testing of novel local treatment modalities that are generated in the microbiology field.
Advertisement
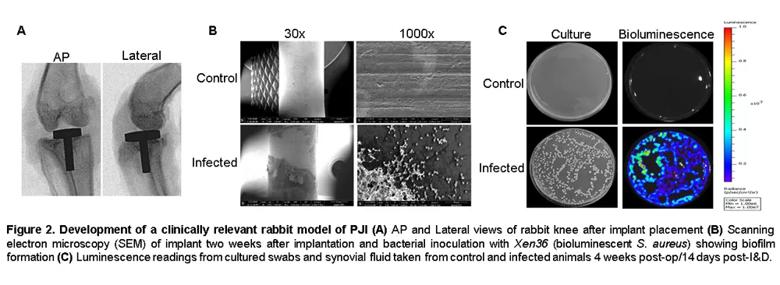
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0a2faf37-4213-4a9b-9082-74cdfe088727/19-ORT-1460-PJI-CQD-Inset-2_jpg)
Dr. Visperas is a Research Coordinator, Department of Orthopaedic Surgery; Dr. Piuzzi is Associate Staff, Department of Orthopaedic Surgery; Mrs. Klika is a Research Program Manager, Department of Orthopaedic Surgery; Dr. Samia is Associate Professor, Department of Chemistry, CWRU; and Dr. Higuera-Rueda is Chairman, Department of Orthopaedic Surgery, Cleveland Clinic Florida
1. Kapadia BH, et al. eriprosthetic joint infection. The Lancet. 2016;387(10016):386-394.
2. Parvizi J, Aggarwal V, Rasouli M. Periprosthetic joint infection: Current concept. Indian Journal of Orthopaedics. 2013;47(1):10.
3. Tande AJ, Patel R. Prosthetic Joint Infection. Clinical Microbiology Reviews. 2014;27(2):302-345.
4. Badarudeen S, et al. Complications After Revision Total Hip Arthroplasty in the Medicare Population. The Journal of Arthroplasty. 2017;32(6):1954-1958.
5. Jafari SM, Coyle C, Mortazavi SMJ, Sharkey PF, Parvizi J. Revision Hip Arthroplasty: Infection is the Most Common Cause of Failure. Clinical Orthopaedics and Related Research®. 2010; 468(8):2046-2051.
6. Mortazavi SMJ, Schwartzenberger J, Austin MS, Purtill JJ, Parvizi J. Revision Total Knee Arthroplasty Infection: Incidence and Predictors. Clinical Orthopaedics and Related Research®. 2010; 468 (8): 2052-2059.
7. Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic Burden of Periprosthetic Joint Infection in the United States. The Journal of Arthroplasty.2012;27(8).
8. Zmistowski B, Parvizi J. A quarter of patients treated for PJI dead within 5 years. Orthopedics Today. https://www.healio.com/orthopedics/infection/news/print/orthopedics-today. Published December 17, 2012.
9. Flemming HC, Wingender J. The biofilm matrix. Nature Reviews Microbiology.2010;8(9):623-633.
10. Mah TFC, O’Toole GA. Mechanisms of biofilm resistance to antimicrobial agents. Trends in Microbiology. 2001.
11. Gatin L, Saleh-Mghir A, Massin P, Crémieux AC. Critical analysis of experimental models of periprosthetic joint infection. Orthopaedics & Traumatology: Surgery & Research. 2015;101(7):851 855.
12. Carli A, et al. Developing a Clinically Representative Model of Periprosthetic Joint Infection. The Journal of Bone and Joint Surgery. 2016;98(19):1666-1676.
Advertisement
Advertisement
Biologic approaches, growing implants and more
Study reports zero infections in nearly 300 patients
How to diagnose and treat crystalline arthropathy after knee replacement
Study finds that fracture and infection are rare
Center will coordinate, interpret and archive imaging data for all multicenter trials conducted by the foundation’s Osteoarthritis Clinical Trial Network
Reduced narcotic use is the latest on the list of robotic surgery advantages
Cleveland Clinic specialists offer annual refresher on upper extremity fundamentals
Cleveland Clinic orthopaedic surgeons share their best tips, most challenging cases and biggest misperceptions