An expert reflects on technical advances and rising success rates
Coronary chronic total occlusions (CTOs) have been described as the last frontier of interventional cardiology. Despite the complexity of these lesions, recent years have seen rising rates of procedural success without offsetting compromises in safety.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In a recent episode of Cleveland Clinic’s “Cardiac Consult” podcast, interventional cardiologist Jaikirshan (Jay) Khatri, MD, explains to podcast host Steven Nissen, MD, some of the reasons why, along with related issues, including:
Click on the player below to listen to the 14-minute podcast now, or read on for an edited transcript of the podcast’s centerpiece discussion of recent advances in the management of CTOs.
Dr. Nissen: I understand that there have been dramatic improvements in success rates in treating CTOs due to advanced crossing strategies. Can you help us understand some of the things you and others are now doing?
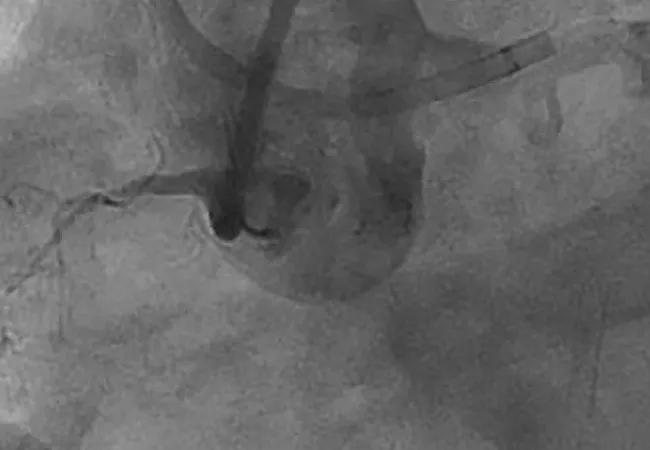
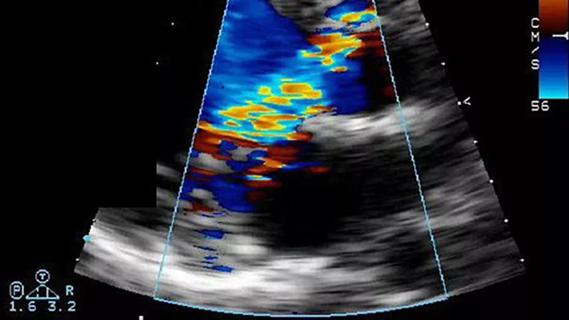
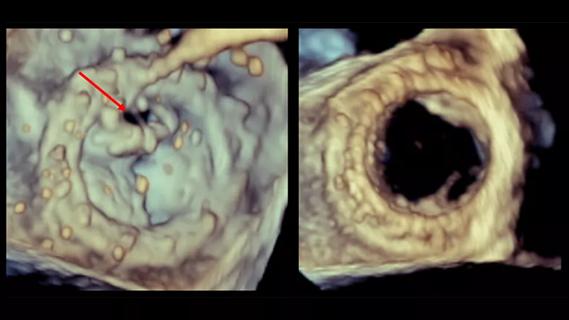
Dr. Khatri: The technique that everyone is most familiar with now is using retrograde collaterals to advance wires to the distal target and then advancing wires to the retrograde system to meet up with the antegrade wires.
Dr. Nissen: So you come from both sides and meet in the middle?
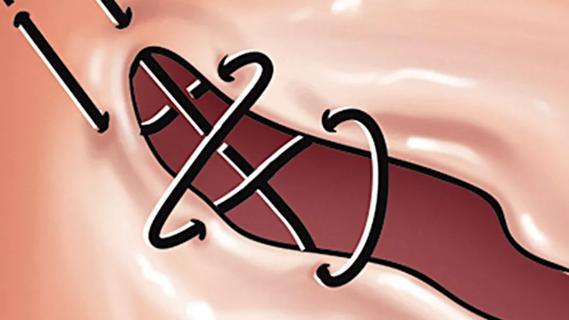
Dr. Khatri: Yes, so you hit the front door and the back door, so to speak, and meet in the middle. Beyond that there are advanced antegrade techniques where we dissect along the artery and then use specialty balloons to reenter the artery distally.
Dr. Nissen: It’s interesting, because in the early era we were trained to do everything we could not to go subintimal, yet now you deliberately go subintimal.
Advertisement
Dr. Khatri: Yes, I live in the subintimal space.
Dr. Nissen: Exactly. Please describe how that procedure works. A lot of people who don’t do this are probably going to be a bit surprised at what operators like you do.
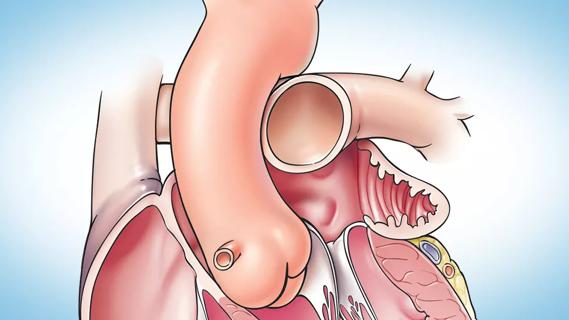
Dr. Khatri: I suppose it is a paradigm shift, as you said, in terms of what an interventional cardiologist does. We are purposely advancing guidewires into the subintimal space on both the antegrade side and the retrograde side because we know that if we’re in the subintimal space, we’re unlikely to perforate, we’re unlikely to enter the pericardium, and we can make connections between the antegrade and retrograde gear.
Dr. Nissen: I would think that getting into the subintimal space would increase the likelihood of perforating the artery.
Dr. Khatri: If one is using the wrong equipment, that’s correct, but there are specialty techniques and wires that we use to traverse the subintimal space in a safe way and make connections.
Dr. Nissen: So you get the wire in the subintimal space. Does it somehow exit later on into the true lumen?
Dr. Khatri: Yes. It either fortuitously reenters the true lumen or you make it enter the true lumen. After that it’s a matter of connecting the dots. Once we have a connection made between the proximal and the distal bed, we can either perform the entire procedure through the antegrade system or use a wire that’s entirely externalized. So it goes in one way and out the other way through the heart, and we use that to deliver our stents.
Advertisement
Dr. Nissen: Okay. Given that you’re in a space where there’s not endothelium, how does the stent reendothelialize?
Dr. Khatri: That’s a scenario that has been studied pretty extensively at this point. It turns out that the data at 12 months and even longer show very good primary patency rates. So it does endothelialize, and some of the reason probably goes back to the IVUS work that you were responsible for showing that outcomes are better if you can expand the stent and appose it to the walls appropriately. So if you are in the subintimal space, which is very compliant, it’s easy to expand stents and easy to appose to the wall. In contrast, it might not be quite as easy in an atherosclerotic segment. That may be part of why this works so well, although we don’t have the evidence for that yet.
Dr. Nissen: Okay, suppose you’ve got a nice big lumen. For how long do you give dual antiplatelet therapy?
Dr. Khatri: We use the standard recommendations for stable patients undergoing coronary intervention, which seem to be diminishing in duration as we get more comfortable with third-generation drug-eluting stents.
Dr. Nissen: In the contemporary era with a really good operator, what should we expect the one-year patency rate to be?
Dr. Khatri: It should be pretty comparable to what we get with standard percutaneous coronary intervention.
Dr. Nissen: That represents an enormous advance over what it used to be. Does it matter how you get at it, whether retrograde or antegrade?
Dr. Khatri: There’s not much differentiation in terms of how we cross. The real issue is the incidence of complications, which is something we’re starting to understand a little better. Complications are higher with a retrograde approach as well as with subintimal dissection re-entry techniques.
Advertisement
Dr. Nissen: What are the complications you worry about most?
Dr. Khatri: The biggest worry is side-branch loss and periprocedural myocardial infarction because of long-term implications for the patient. But there are also technical issues that can happen during the procedure, like rupture of a collateral, pericardial effusions or tamponade. There can even be mechanical complications related to intramural hematoma that are created by these advanced techniques.
Dr. Nissen: What kind of perforation rate is considered acceptable in this setting?
Dr. Khatri: That has been relatively underreported. Some recent registry data indicate that in busy centers involved in multicenter registries it’s around 3%.
Dr. Nissen: Of course, these are patients whose symptoms are making them miserable, who may have trouble walking to the bathroom without chest pain, so they tend to be willing to accept a 3% risk.
Dr. Khatri: Yes, and on top of that, the 3% rate is from very high-volume, experienced operators. It’s not from an all-comer dataset.
Dr. Nissen: So this is no space for amateurs, right?
Dr. Khatri: It’s a very difficult procedure and the stakes are high, so it requires a real level of comfort, including comfort with how to manage the complications, because complications will occur.
Dr. Nissen: At a major center with a skilled operator, how often is it just not possible to get across the occlusion? What is the true failure rate?
Dr. Khatri: With the kind of patients we see here, many of whom have already had failed attempts with experienced operators at other centers, our success rate is approximately 87%.
Advertisement
Dr. Nissen: Given that these are patients whose quality of life is being very significantly impaired, that is quite good.
Dr. Khatri: It is. And with the right patient who understands the risk of the complications, it’s a very gratifying procedure to undertake even if it’s not always successful.
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
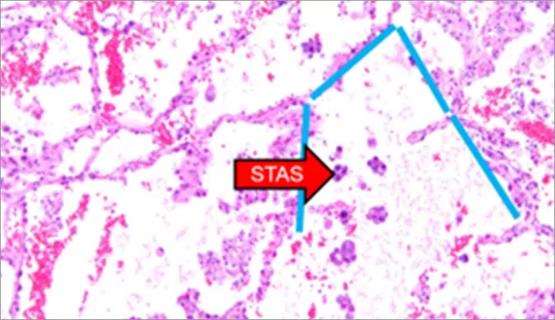
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable