Case presentation explains surgical treatment
It is estimated that 10 to 20 percent of women will undergo a surgical procedure for stress urinary incontinence (SUI) in their lifetime. The synthetic midurethral sling is considered the current gold-standard surgical treatment for SUI.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
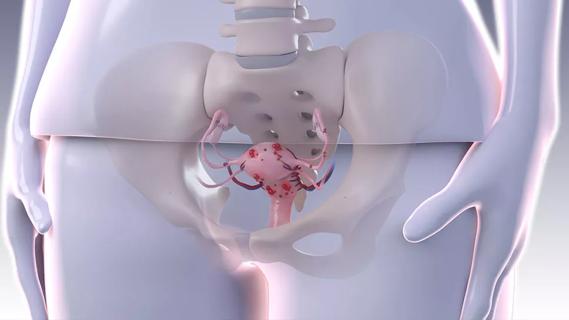
Urethral complications due to synthetic midurethral sling are uncommon (0.4 to 4 percent). Causes of urethral perforation after synthetic midurethral sling include unrecognized intraoperative entry into the urethra or excessive sling tension, which may lead to erosion over time. Currently, there is no consensus as to the surgical management of urethral complications. If urethral perforation occurs, transvaginal and endoscopic removals are options. Flaps may or may not be used, and surgeons are divided on the feasibility and safety of concomitant incontinence procedures such as a pubovaginal sling. An individualized approach is used based on patient presentation and surgeon expertise.
In this video, urological surgeon Howard Goldman, MD, of Cleveland Clinic’s Glickman Urological & Kidney Institute demonstrates the pre-procedure patient evaluation and surgical technique of transvaginal sling removal from the urethra and concomitant urethral reconstruction. The patient as a 66-year-old woman with a history of anterior and posterior colporrhaphy and a retropubic, midurethral sling 12 years prior. The patient reported difficulty voiding since the time of the surgery, saying that she had to stand and bend over in order to urinate. Physical exam revealed tenderness to palpation of the anterior vaginal wall and no mesh extrusion.
In the past, she had undergone three prolapse repairs, the last one in 2005 with a concomitant vaginal hysterectomy. During an outpatient cystourethroscopy, the bladder was normal, but there was a urethral perforation distal to the bladder neck, and her urodynamics were consistent with obstruction.
Advertisement
The surgery was the subject of a presentation at the American Urological Association’s 2016 annual meeting.
Advertisement
Advertisement
Counseling and careful surgical considerations are key

Deprivation is linked to impaired glucose intolerance and racial disparities

Perioperative prophylaxis and class III obesity

Artesunate ointment is safe well and tolerated patients with vulvar intraepithelial neoplasia

Endoscopic balloon dilation during pregnancy helps optimize outcomes

Researchers examine waste and implore colleagues to take action

Mode of delivery does not affect patient satisfaction