Analysis of large re-replacement surgery cohort pinpoints key characteristics
Advanced symptoms, renal dysfunction and heart block are the leading risk factors to consider when selecting candidates to undergo transcatheter valve-in-valve therapy for a failed bioprosthetic mitral valve.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So conclude the authors of a large Cleveland Clinic analysis of contemporary outcomes of mitral valve re-replacement surgery for bioprosthetic structural valve deterioration conducted to set a benchmark for transcatheter therapies.
“Data from the STS Adult Cardiac Surgery Database show an increasing shift toward use of bioprosthetic valves and a decrease in the age of patients undergoing mitral valve replacement,” says A. Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic and a coauthor of the study, which was presented at the AATS annual meeting on May 1. “These trends inevitably will lead to more patients developing structural valve deterioration. As enthusiasm grows for valve-in-valve transcatheter mitral valve replacement for degenerated bioprostheses in highly selected patients, establishing a framework for outcomes and risk factors based on surgical mitral valve re-replacements is important.”
To that end, Dr. Gillinov and colleagues reviewed all 1,090 mitral valve re-replacement surgeries performed at Cleveland Clinic from January 1990 to January 2017. Of these, 462 surgeries involved explantation of a bioprosthetic valve for structural deterioration, which was the focus of the study.
Among these 462 cases, the dominant characteristic of the deterioration was regurgitation in 81 percent of cases, with stenosis involved in 35 percent of cases. Most patients were symptomatic, and 49 percent were in New York Heart Association (NYHA) functional class III or IV. Mean patient age at mitral valve re-replacement was 67 years, and the median interval between bioprosthesis implantation and re-replacement was 10 years.
Advertisement
End points included in-hospital mortality and morbidity as well as time-related mortality. Risk factors were assessed using multivariable nonproportional hazards analysis. Median follow-up was 5.7 years, with 10 percent of survivors followed at least 19 years.
Hospital mortality for mitral valve re-replacement was 6.1 percent. Long-term survival rates were as follows:
Leading risk factors for all-cause mortality early after re-replacement were as follows:
Leading risk factors for all-cause long-term mortality were as follows:
Dr. Gillinov notes that surgical re-replacement has been the standard treatment strategy for bioprosthetic mitral valves that develop severe stenosis or regurgitation due to prosthesis deterioration. He adds, however, that this approach carries heightened risks in patients with significant comorbidities or in poor clinical condition, as well as when procedural complexity is high.
“Transcatheter valve-in-valve therapies are evolving as an alternative to surgical re-replacement in patients who are at high surgical risk,” he says. “We believe the results from our surgical analysis help set a benchmark for transcatheter therapy as it continues to evolve. Our findings align with previous reports and indicate that risk factors associated with early mortality — higher NYHA class, renal dysfunction and heart block — are useful for identifying high-risk patients who may be candidates for transcatheter therapies.”
Advertisement
The study will be submitted for publication soon.
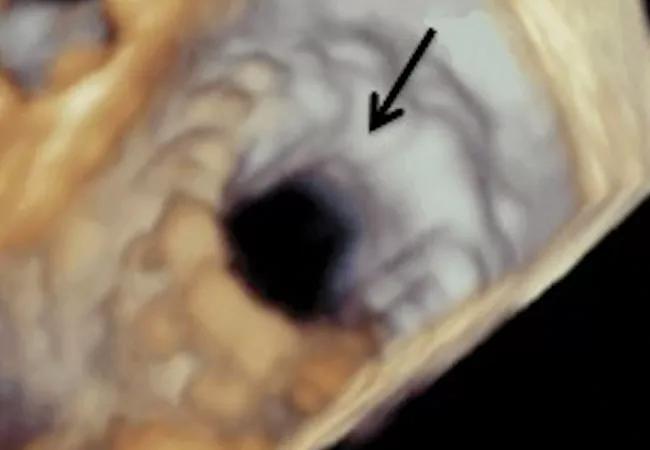
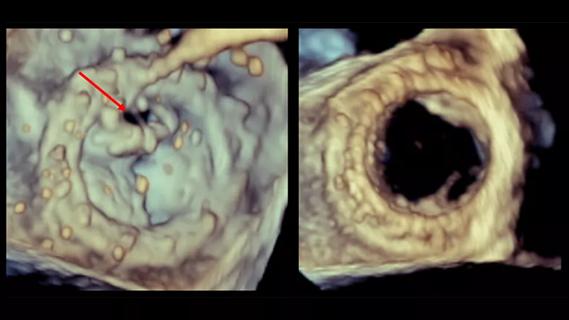
Image at top: 3D transesophageal echo view of an open mitral valve following valve-in-valve placement. Reprinted from Cleveland Clinic Journal of Medicine (2016;83[suppl2]:S10-S17).
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable