TOS subtype matters a lot, as do anatomic findings
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 53-year-old right-handed man presents to Cleveland Clinic’s Department of Vascular Surgery for a consult evaluation for thoracic outlet syndrome. He has a history of chronic upper back pain (> 4 years), neck pain (> 3 years), and left arm pain and discomfort (3 years).
Because his symptoms improve with his left arm at rest, he avoids using it as much as possible and has had resultant muscle wasting. He complains of burning, stabbing, throbbing pain in the left armpit that travels down to the fourth and fifth fingers, as well as in the proximal left palm. He reports having intermittent numbness in his left arm, hand and fingers since childhood, along with muscle wasting in his left hand.
The patient reports that doing overhead work for prolonged periods is an exacerbating factor. As an inspector at a steel company, he repeatedly picks up 2 to 10 pounds every day — a task for which he uses his right arm. He avoids using his left arm for any prolonged activity above shoulder level (e.g., holding the telephone to his ear, hair-washing, holding the top of the steering wheel).
He has undergone physical therapy and taken pain medications, without marked relief. He reports that recent lidocaine injections to his cervical neck were helpful.
He has undergone orthopaedic and neurologic evaluation. Previous diagnostic testing included a spinal X-ray, MRIs of the spine and shoulder, and electromyography testing. Of note, he was found during workup to have a full left C7 cervical rib, a rare anatomic variation. While 0.75 percent of the population has a complete or incomplete cervical rib, many have only an extra length, whereas this patient has a full rib with an articulating joint in the middle.
Advertisement
Thoracic outlet syndrome (TOS) involves upper extremity symptoms due to compression of the neurovascular bundle at the superior thoracic outlet by any of various structures in the area just above the first rib and behind the clavicle.
Among the three TOS subtypes — neurogenic, venous and arterial — neurogenic accounts for about 96 percent of cases, followed by venous (3 percent) and arterial (1 percent).
When a cervical rib is present along with signs and symptoms of TOS, it is most commonly a case of neurogenic TOS, which was my diagnosis for this patient. While no one test or physical finding can definitively diagnose TOS, I based this diagnosis on the clinical history, physical exam findings and elimination of other diagnoses.
I recommended the clear course of action — decompression surgery to remove the cervical rib — and the patient agreed. The surgical approach can be supraclavicular or transaxillary and is decided at the surgeon’s discretion based on technical experience, presence/absence of a cervical rib, involvement of the upper brachial plexus cords and the patient’s surgical history.
This neurogenic case called for a supraclavicular approach, due to the presence of the cervical rib. If the surgery had been for venous TOS or a milder neurogenic case, I would have used a transaxillary approach.
Under a supraclavicular approach like this, a neck roll is used to extend the shoulders and the head is rotated to the contralateral side. An incision is made above the clavicle in a parallel fashion from the lateral head of the sternocleidomastoid toward the shoulder. The platysma is transected and tissues dissected to identify the scalene fat pad. The fat pad should be mobilized in a superior lateral fashion, with care taken to protect the thoracic duct. This allows exposure of the anterior scalene muscle. The phrenic nerve will be seen from superior lateral to inferior medial and should be dissected and protected.
Advertisement
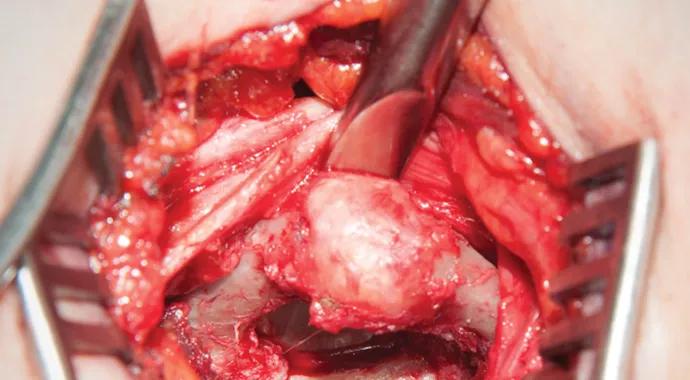
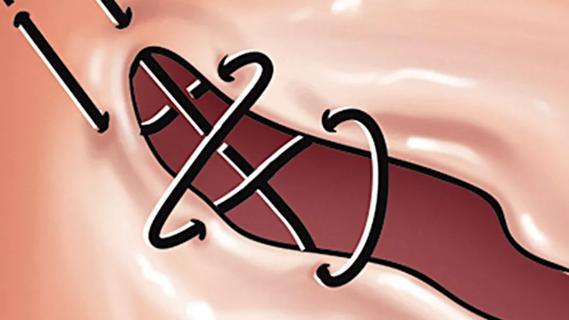
The anterior scalene is partially resected, allowing visualization of the subclavian artery, which can be mobilized to improve exposure of the rib. The brachial plexus will be seen lateral to the artery and should be dissected from the surrounding tissue. The first rib will lie underneath these structures and can be manually palpated. The cervical rib lies more superiorly, and with retraction of structures, it can be cleared circumferentially from its posterior attachment (Figure 1). The rib or ribs are then removed en bloc (Figures 2 and 3).
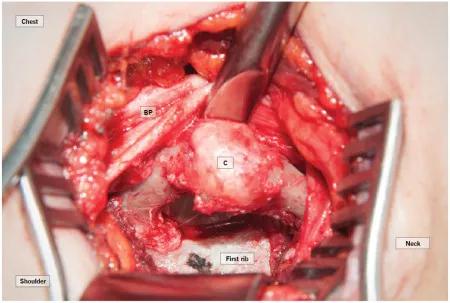
Figure 1. Retraction of the brachial plexus (BP) in the case patient showing the cervical rib (labeled “C”) and articulating joint. Note the first rib more posteriorly.
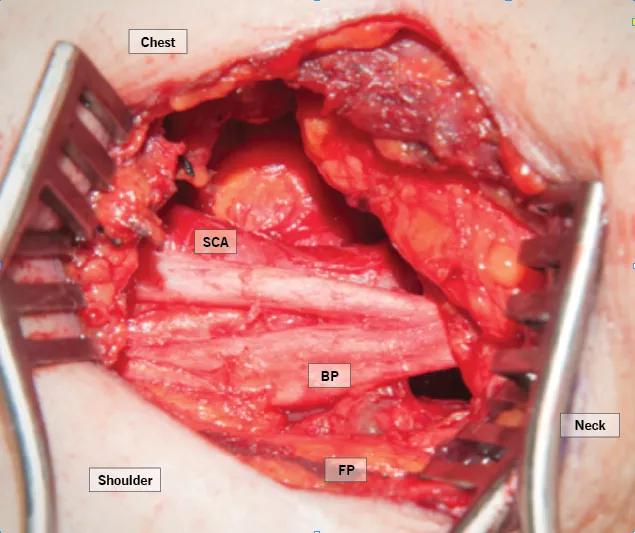
Figure 2. The brachial plexus (labeled “BP”) back in normal position after resection of the cervical rib and first rib with associated scalene muscle attachments. (SCA = subclavian artery; FP = fat pad)

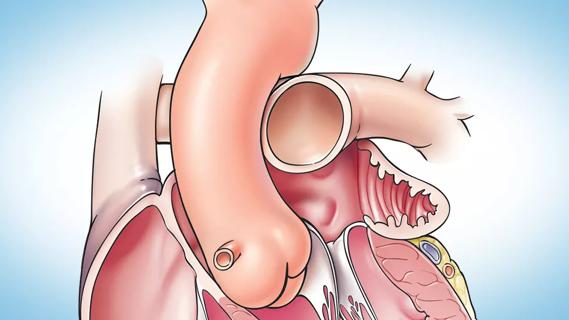
Figure 3. En bloc resection of the first rib and attached cervical rib. Arrow notes the articulation joint in the cervical rib.
The postoperative course includes a 24-hour observation period, with a combination of NSAIDs and narcotics for pain control. We require postoperative physical therapy for all surgery patients.
The patient is now one month postop and showing improvements, including in all ulnar-based symptoms. His shoulder pain has improved, pain has decreased in his neck with the movement of his head and he is now starting physical therapy. Because of the severity of his preoperative symptoms, he will likely have a prolonged recovery (two to three months) with nerve recovery continuing for six to 12 months.
Advertisement
While TOS is a fairly unusual specialty area within vascular surgery, it’s an important one — and one in which several Cleveland Clinic vascular surgeons have extensive experience. My own caseload has grown to approximately 30 TOS surgeries per year, with a mix of neurogenic and venous cases.
Because these procedures can affect arm function, TOS cases tend be highly litigious, which makes surgeon skill even more important.
Many patients referred to our center have had symptoms for nine to 18 months or more, seen various specialists and undergone multiple diagnostic tests, many of them unremarkable. Because of this widespread delay in diagnosis and the lack of confirmatory tests — as well as the fact that earlier interventions tend to be most successful — we urge colleagues to refer whenever there is a suspicion for TOS.
Special attention to the history and symptoms is crucial to diagnosis of TOS. Symptoms often overlap with more common diagnoses, including cervical spine disorders, rotator cuff or shoulder injury, ulnar nerve entrapment and carpal tunnel syndrome. These diagnoses must be excluded, often through neurologic and orthopaedic evaluations.
Diagnosing arterial and venous TOS is sometimes easier than diagnosing neurogenic disease, due to arm findings related to chronic injury to vessels. However, patients with extensive and prolonged symptoms of neurogenic TOS may have an element of sympathetic nerve involvement with color changes, swelling and mottling, which can be confused with arterial or venous TOS.
Advertisement
Only 20 to 30 percent of patients with TOS need surgical treatment, so evaluation includes careful consideration of whether surgery will benefit the patient. Surgery primarily involves resection of the rib(s) and associated scalene muscles and release of scar tissue surrounding the neurovascular bundle.
Patients with a cervical rib (like this one) often require surgical treatment, though many other neurogenic patients achieve satisfactory relief from TOS-specific physical therapy and medical management. Since most cases of venous or arterial TOS present with symptoms, surgery is first-line therapy in these patients.
Surgical outcomes are generally positive for well-selected patients. With judicious patient selection and proper patient adherence to physical therapy and movement restrictions until pain is resolved, surgical treatment of TOS can lead to improvement in about 80 percent of patients.
Dr. Kelso is a surgeon in the Department of Vascular Surgery.
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
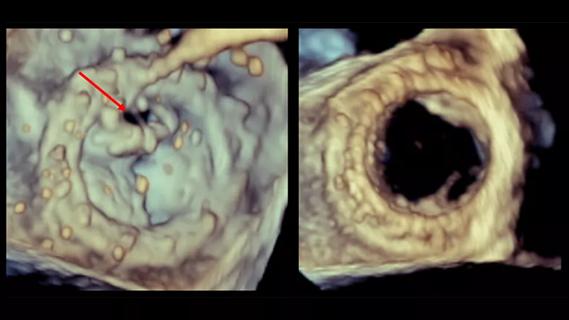
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
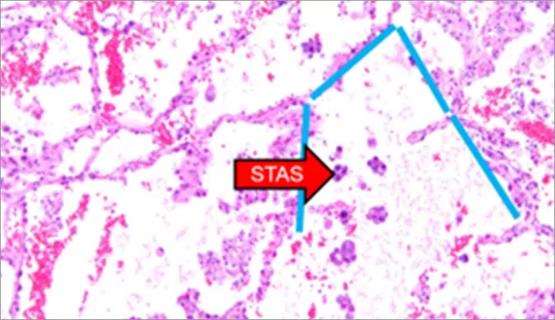
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
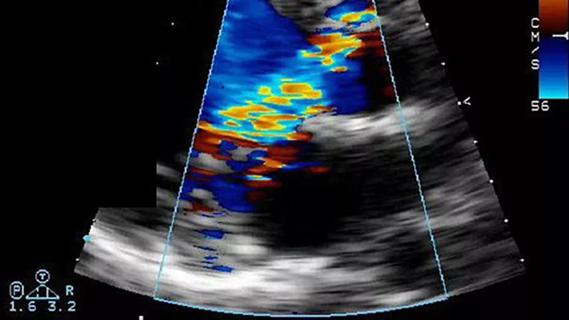
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable