The stakes of — and reasons behind — the ‘cult of statin denial’
Unfounded public distrust of statin drugs contributes to “shockingly low” statin adherence rates and is fueled by a proliferation of online misinformation about statins and cholesterol. So argues Cleveland Clinic Cardiovascular Chair Steven Nissen, MD, in an editorial in Annals of Internal Medicine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This infographic lays out some interesting numbers behind this phenomenon, which Dr. Nissen dubs the “cult of statin denial.” For more detail, including how physicians can counter this trend, see this related post and Dr. Nissen’s full editorial.
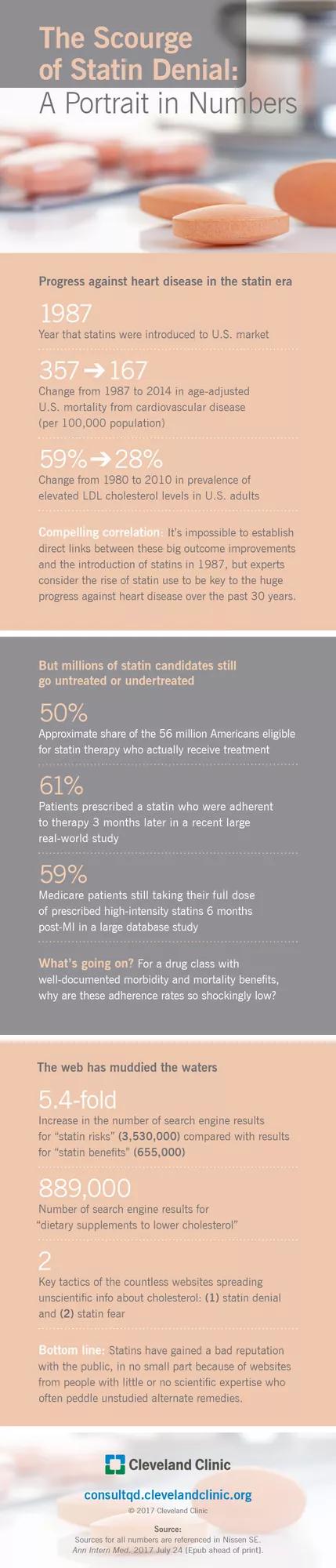
“Statins have developed a bad reputation with the public, a phenomenon driven largely by proliferation on the Internet of bizarre and unscientific but seemingly persuasive criticism of these drugs,” writes Dr. Nissen. As one sign of the extent of the phenomenon, he cites these sobering stats: The 655,000 search engine results yielded by the term statin benefits are utterly dwarfed by the 3,530,000 results produced by the term statin risks.
“We are losing the battle for the hearts and minds of our patients to Web sites developed by people with little or no scientific expertise,” he continues, noting that these sites primarily propagate one or both of two key notions:
Far too often the result is that patients discontinue their statin therapy or forgo it in the first place, resulting in “shockingly low” statin adherence rates that often have grave consequences, Dr. Nissen argues.
This leads him to conclude that “[p]assive acceptance of harmful pseudoscience is not an option.” He argues that thoughtful physicians “must work together to educate the public and enlist media support, and we must take the time to explain to our patients that discontinuing statin treatment may be a life-threatening mistake.”
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable