A potentially definitive repair in a young woman with multiple prior surgeries
A woman in her 30s with severe dyspnea was referred to Cleveland Clinic from out of state for aortic valve reoperation. Despite her young age, she had a history of two previous cardiac surgeries related to genetic predisposition for coronary artery disease and congenital aortic valve disease. She had undergone complete coronary revascularization using both internal mammary arteries. A few years later, her aortic valve and ascending aorta were replaced. The following year, she underwent surgery for deep sternal wound infection, likely resulting from the aortic valve surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Upon arrival at Cleveland Clinic, the patient underwent cardiac catheterization. It revealed a high gradient across her aortic valve, indicating that her 19-mm bioprosthetic valve was too small. After a CT scan found no lingering infection in her chest, she was cleared for surgery.
Consideration was given to replacing the aortic valve with a tissue or mechanical prosthesis in a minimally invasive or open surgical procedure. However, in view of the patient’s age, gender and cardiac history, that option was rejected in favor of the Ross procedure.
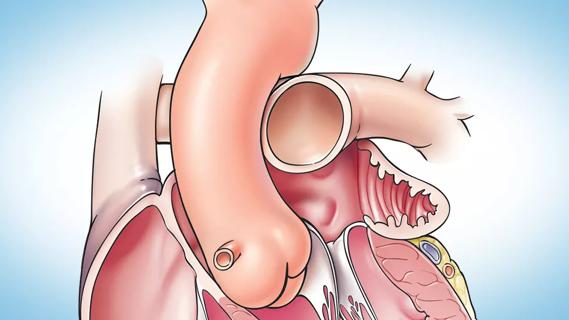
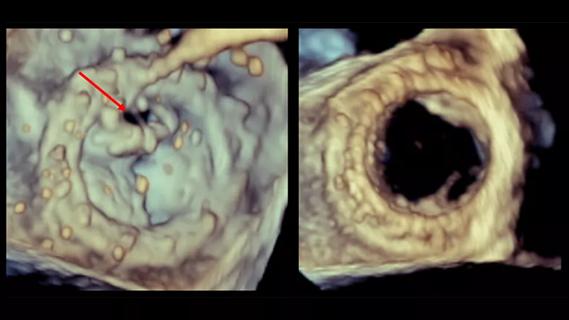
A surgical team led by Gosta Pettersson, MD, PhD, removed the patient’s aortic prosthesis, harvested the pulmonic valve and reimplanted it in the aortic position. This was reinforced with native aortic root tissue for support, and the pulmonic valve was replaced with a homograft (Figure).
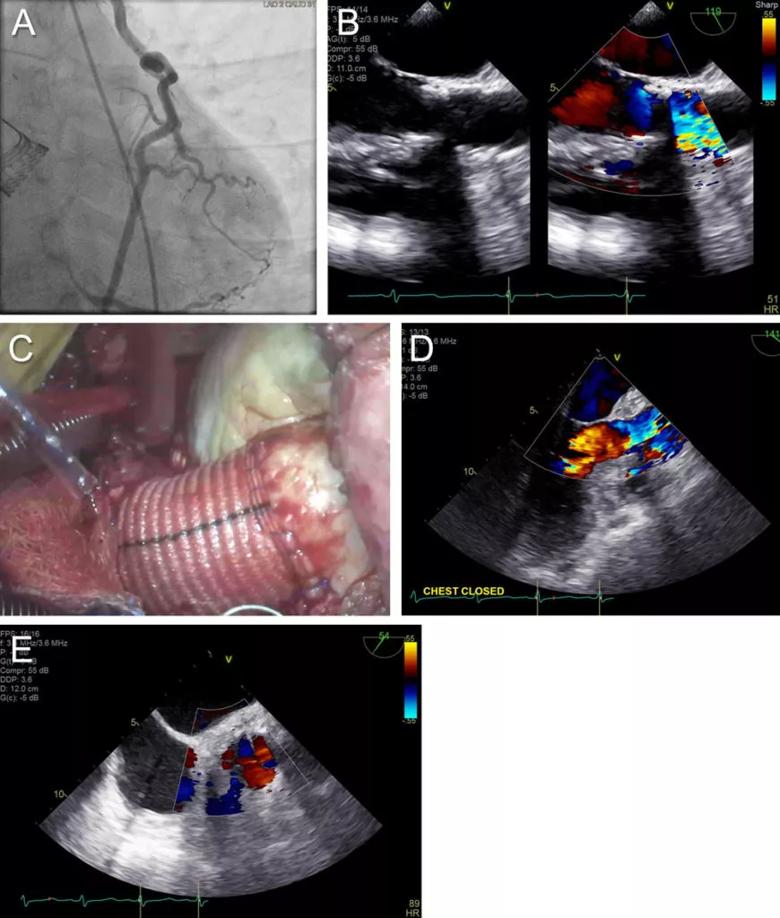
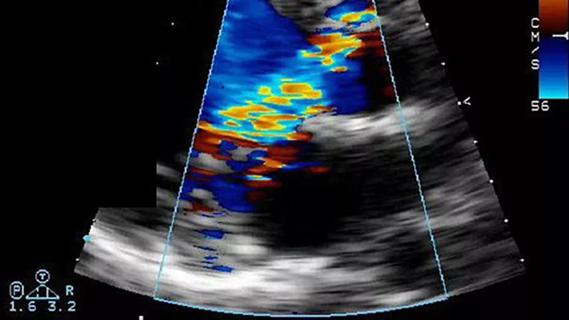
Figure. (A) Still from the patient’s coronary catheterization showing the coronary artery dependence on mammary artery bypass with connection to multiple branches. (B) Preoperative echocardiogram stills of the aortic valve with color Doppler to the right showing high velocity and turbulence across the valve. (C) Photo of the completed surgery. The foreground shows the autograft (patient’s pulmonary valve) in the aortic root extended with a vascular graft. In the background is the homograft replacing the harvested pulmonary valve. (D and E) Postoperative echocardiogram stills showing a well-functioning aortic valve (pulmonary autograft) without any significant gradient or regurgitation.
Advertisement
After an unremarkable recovery, the patient returned home to the care of her local cardiologist. Six months later, she reported mild tenderness in her sternum and slight dyspnea that did not prevent her from going about her daily life.
Although performed relatively infrequently, the Ross procedure provides optimal hemodynamics, has very good longevity (a 20-year reoperation-free rate of 80% or more) and is associated with low risk of valve infection.
Ross candidates are young and, as such, reluctant to accept a mechanical valve requiring lifelong anticoagulation, and they are not well matched to a tissue valve prosthesis, which may not last that long in young people. If AVR with a tissue valve prosthesis is still pursued, the shorter life span of the prosthesis in this age group makes it likely that multiple reoperations will be needed over the patient’s lifetime.
It is important to also note that more than half of this young population are women of childbearing age, and a mechanical prosthesis would greatly increase the maternal and fetal risks during pregnancy due to the need for systemic anticoagulation.
An option in some patients to minimize the total number of redo median sternotomies is transcatheter aortic valve replacement (TAVR), which is not feasible in all patients, depending on coronary artery position relative to the prosthetic valve, annular size and risk of patient-prosthesis mismatch.
Implanting a tissue valve via TAVR to delay the need for another open surgery was not an option in this patient, Dr. Pettersson observes, because of the small size of the prosthesis and because it would have further complicated future open surgery.
Advertisement
The Ross procedure makes all of these issues moot, Dr. Petterson notes. “Replacing the aortic valve with the pulmonary valve puts the best valve in the most important position,” he says. “Shifting the pulmonary valve to the aortic location also gives you a valve with the same-size opening, which prevents a patient-prosthetic mismatch, as had been the case after this patient’s earlier AVR.”
A pulmonary autograft in the aortic position requires external support to prevent dilatation under the high systemic pressures on the left side of the heart. Having performed approximately 250 Ross procedures in his career, Dr. Pettersson has found that supporting the autograft by surrounding the valve with native aortic root tissue is the ideal solution, although not the only option.
“The pulmonary valve can also be supported by a Dacron graft or felt strips, but I favor Dr. Pettersson’s method of using native aortic root tissue because it does not restrict the motion of the pulmonic autograft, and it minimizes the risk of infection,” notes cardiothoracic surgeon Shinya Unai, MD, who worked with Dr. Pettersson on this case.
A complex and technically challenging operation, the Ross procedure is best performed by surgeons with expertise in aortic root surgery.
“We perform many complex root surgeries and consider this a baseline skill for doing Ross procedures,” says Dr. Unai. “The techniques required for the Ross are similar: You need experience and familiarity with root anatomy and replacement, as well as with homograft root replacement. This is what translates to success in the Ross operation.”
Advertisement
Dr. Pettersson adds that this is particularly true in a reoperative context. “Reoperations require dissection of the heart and, in our case, dissection of the coronary grafts that are attached to the root, so intimate knowledge of root anatomy is essential,” he says. “In this patient, preventing damage to the bypass grafts was a major concern, since her own arteries were not good, and her internal mammary arteries had already been used.”
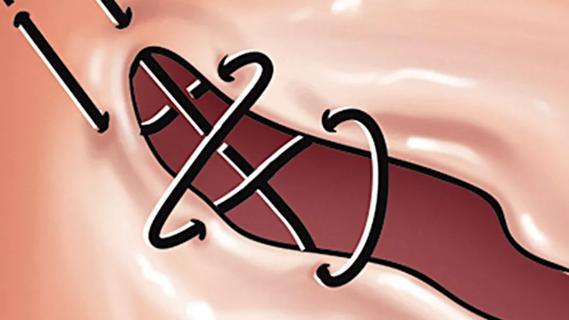
Although the Ross procedure does introduce the potential of damaging a second valve, the likelihood of such damage is very low if the pulmonary valve is treated with care. “The walls of the autograft are thin, so one must be gentle and meticulous in suturing,” says Dr. Pettersson.
A well-done Ross procedure allows young patients to resume a normal, healthy lifestyle (including competitive sports) without experiencing symptoms or worrying about the need for another valve replacement.
“The Ross procedure remains a great option in young patients, and although active infection was not an issue in this patient, she had had infectious complications in the past,” says Cleveland Clinic cardiologist Paul Cremer, MD, who helped manage the patient’s care. “I have also had good results referring certain younger patients for the Ross procedure in the setting of bicuspid aortic valve endocarditis.”
Cleveland Clinic’s outcomes with the Ross procedure are excellent, and Drs. Pettersson and Unai expect this patient to continue that trend. Nevertheless, she may potentially require a future operation for either the autograft, the homograft or both, as the Ross procedure carries an approximate 20% risk of reintervention by 20 years. “Homograft dysfunction can most often be addressed percutaneously,” Dr. Pettersson notes. “Ross reversal is an option for patients who get in trouble with two valves.”
Advertisement
“Transcatheter pulmonary valve replacement to address the failing pulmonary autograft is a relatively lower-risk procedure with short hospital stay and quick recovery,” adds Joanna Ghobrial, MD, MS, a Cleveland Clinic cardiologist not involved in the current case. ”If needed, it can obviate the need for redo surgery or buy the patient time before the need for any redo surgery.”
“We hope this is the last heart operation this patient will need,” adds Dr. Unai.
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
Large retrospective study supports its addition to BAV repair toolbox at expert centers
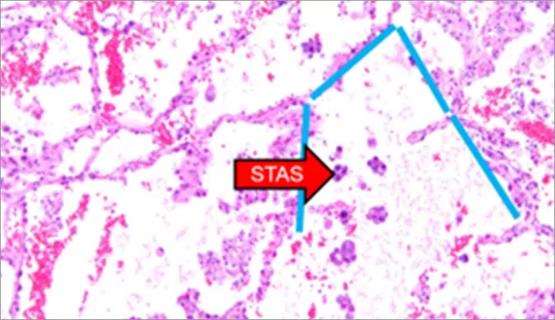
Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture
Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age
Provides option for patients previously deemed anatomically unsuitable