Best Practices Mitigate Catastrophic Risk

By Russell DeMicco, DO, and Garett Helber, DO
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There is ongoing debate over using a particulate versus a nonparticulate corticosteroid for epidural steroid injections (ESIs) as a treatment for radicular pain caused by disk herniation and/or spinal stenosis.
ESIs are known to be associated with both minor and major complications, from severe neurological deficits caused by spinal cord infarct and stroke to minor side effects, including neurogenic/vagal reaction, postdural puncture headache (PDH) and pain exacerbation. Although severe neurological deficits caused by ESIs are rare, the disability associated with them could be catastrophic.
These risks exist even when ESIs are performed by experienced proceduralists.
Given this background, both the proceduralist and the referring physician should fully understand how potential complications might occur in order to recommend the optimal treatment plan for each patient.
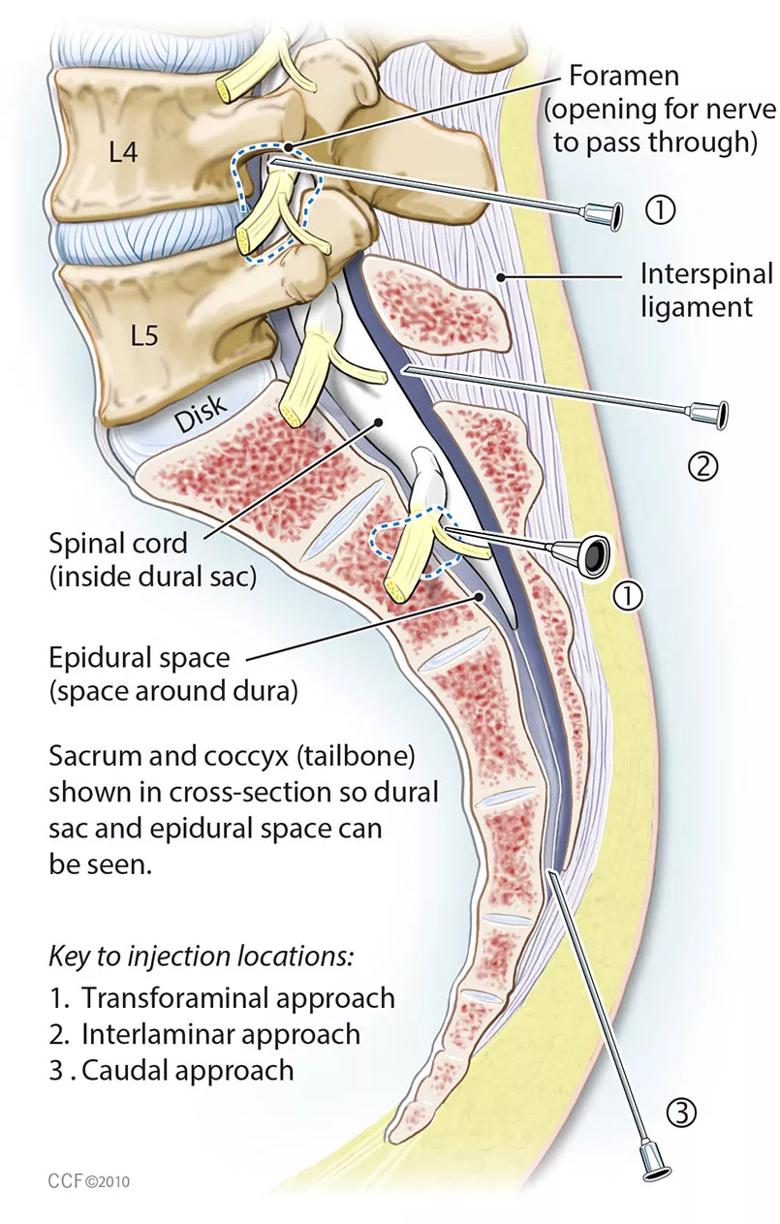
Along the cervical, thoracic and lumbar regions of the spine, corticosteroid administration can be achieved either via the interlaminar or transforaminal route (figure).
Cervical transforaminal epidural steroid injections (CTESI) can be both diagnostic and therapeutic. The diagnostic utility of cervical interlaminar epidural injections (CESI) compared with CTESI is questionable. For this reason, CESI is often used as a therapeutic modality for those with radicular pain, although both procedures incur risk of spinal cord injury complications.
Injury may occur either from direct trauma (injection to the spinal cord or spinal nerves) or indirect trauma (vascular blockade from a particulate steroid or vasospasm from a nonparticulate stimulus).
Advertisement
Direct trauma is due to intracord injection, hematoma or increased pressure from the injectate. Injury can occur instantaneously if the proceduralist does not recognize abnormal contrast flow patterns under fluoroscopy.
Injury from particulate steroid injection has proved to be the main etiology of spinal cord injury. Animal studies, as well as case reports in humans, have hypothesized that particulate steroids are more likely to lead to spinal cord complications than nonparticulate steroids, due to blocked arterial blood supply to the spinal cord.
Anatomical studies have shown that the vertebral artery and the ascending cervical and deep cervical arteries are proximate during cervical transforaminal injections. Betamethasone has the smallest particles, triamcinolone’s are intermediate and methylprednisolone’s are the largest. With dexamethasone, particulation is not evident, and therefore it is classified as a nonparticulate steroid.
It is possible to cannulate the arteries unintentionally, which can cause dissection, perforation or even something as minute as embolization of an intimal flap. All of these scenarios can result in catastrophic events similar to those that may occur from a particulate stimulus.
Given these potential risks, the realistic goal is to reduce complications, even though 100 percent prevention is, without a doubt, utopian.
The U.S. Food and Drug Administration’s Safe Use Initiative (SUI) convened in 2009 to facilitate collaboration with pain societies. Scientists and clinicians collaborated to set evidence-based clinical guidelines to mitigate catastrophic events associated with ESIs.
Advertisement
The group unanimously agreed on steroid use, making the following comments and recommendations:
There is no clear consensus regarding the use of real-time fluoroscopy and/or digital subtraction angiography. Our institution’s clinical experience has shown that real-time fluoroscopy (when digital subtraction angiography is not available) is capable of preventing neurovascular complications. This is based on the premise that the proceduralist has adequate training in identifying correct needle positioning and contrast flow patterns.
Based on our institutional experience, other recommendations include:
Advertisement
As we move more and more toward evidence-based therapies, it is strongly recommended that a nonparticulate steroid be used for all cervical transforaminal ESIs. If available, digital subtraction angiography should be utilized — or at minimum, real-time fluoroscopy — when performing cervical through lumbosacral injections.
Proper training and experience should be given high priority in the credentialing process, especially for cervical spine injections. Only by following these best practices can we realistically mitigate the risk of these catastrophic injuries.
Beckman WA, Mendez RJ, Paine GF, Mazzilli MA. Cerebellar herniation after cervical transforaminal epidural injection. Reg Anesth Pain Med.2006;31(3):282-285.
Brouwers PJ, Kottink EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001;91(3):397-399.
Dawley JD, Moeller-Bertram T, Wallace MS, Patel PM. Intra-arterial injection in the rat brain: Evaluation of steroids used for transforaminal epidurals. Spine. 2009;34(16):1638-1643.
Derby R, Lee SH, Date ES, Lee JH, Lee CH. Size and aggregation of corticosteroids used for epidural injections. Pain Med. 2008;9(2):227-234.
Dr. DeMicco is a medical spine specialist in the Center for Spine Health, and Program Director, Spine Medicine Fellowship. He can be contacted at demiccr@ccf.org or 216.444.0229.
Dr. Helber is associate staff physician in the Center for Spine Health. He can be reached at helberg@ccf.org or 216.445.6638.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade