Negative antibody testing doesn’t always rule it out
By Ahsan Moosa Naduvil, MD, and Andrew Zeft, MD, MPH
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 17-year-old right-handed female presented to Cleveland Clinic with recurrent complex partial seizures that started at age 14. During seizures, she experienced tingling all over her body followed by confusion and unresponsiveness lasting less than a minute. These episodes were not recognized as seizures until about three years after their onset, when the spells became more intense, with longer periods of unresponsiveness multiple times a week.
She was otherwise healthy, with normal development and no obvious risk factors for epilepsy. Her neurological examination was normal. Six years earlier, at age 11, she had emergency surgery for right ovarian torsion secondary to teratoma.
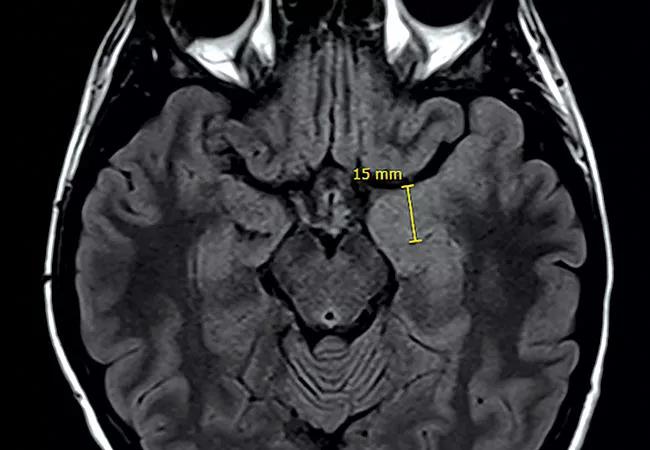
Initial evaluation showed left temporal epileptiform activity on EEG. Brain MRI showed hyperintensity of left mesial temporal structures with enlargement of the left amygdala (Figure, panel A). Despite treatment with levetiracetam, the seizures persisted and she was admitted emergently after a cluster of seizures at school. Five habitual complex partial seizures arising from the left temporal region were captured on video EEG. Oxcarbazepine was added to her treatment regimen. Brain FDG-PET showed focal hypermetabolism in the left amygdala.
In view of her prior history of right ovarian teratoma, further testing was done to rule out paraneoplastic/autoimmune etiology. Testing for antibodies — including anti-N-methyl-D-aspartate receptor (NMDAR) anti-neuronal antibody type 1, anti-glial nuclear antibody type 1, amphiphysin antibody, CRMP-5-IgG and thyroid antibody — in blood and CSF was negative. However, PET and CT imaging of the pelvis showed a tumor in the left ovary.
Advertisement
She underwent removal of a teratoma with a fertility-sparing surgery. Her immunotherapy regimen included a pulse of IV methylprednisolone followed by oral steroids, monthly IV immunoglobulin and two doses of rituximab.
Follow-up brain MRI a year later showed resolution of the left mesial temporal abnormalities (Figure, panel B). Immunotherapy was weaned and discontinued by one year after surgery. After a seizure-free period of one year, levetiracetam was weaned. She had two generalized motor seizures due to nonadherence to her oxcarbazepine therapy. She has since remained seizure-free on oxcarbazepine monotherapy.
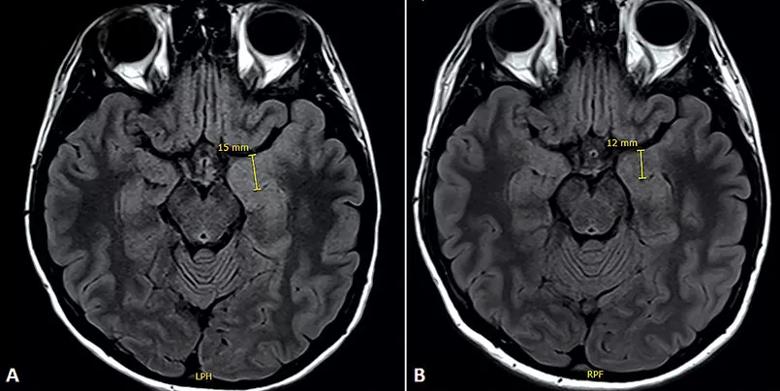
Figure. (A) Axial FLAIR MRI at initial evaluation showing hyperintensity and enlargement of the left mesial temporal region, particularly the amygdala. Effacement of the left temporal horn due to the enlarged amygdala is evident. (B) One year after treatment, the mesial temporal structures and the temporal horns appear symmetrical.
Teratoma-related encephalitis, especially anti-NMDAR encephalitis, is well-documented. Seizures may occur in about 8 percent of patients with NMDAR encephalitis, but isolated presentation with seizures is rare.
Absence of NMDAR antibody in our patient posed a further challenge to confirming the diagnosis. Features supportive of an autoimmune etiology included presence of a tumor known to affect limbic structures, initial swelling and hyperintensity of the medial temporal structures, reversal of these changes with treatment, left amygdala hypermetabolism on PET, and a good, sustained response to treatment.
Advertisement
Prior history of tumors should alert providers to the possibility of a paraneoplastic process. A negative serological test does not exclude a paraneoplastic process. Tumor removal and immunotherapy improve the outcome in treatment-responsive patients.
Autoimmune etiologies in children and adolescents with chronic epilepsy may be underappreciated. Recognizing an autoimmune process as a cause of epilepsy offers opportunities to treat the underlying etiology and potentially cure the disease.
An explosion of information on neuronal autoantibodies in patients with autoimmune and paraneoplastic limbic encephalitis has excited interest in the role of such antibodies in epilepsy. Target antigens to many of these anti-neuronal antibodies are closely linked to epileptogenesis; moreover, seizures are common in autoimmune encephalitis.
Population studies have shown that the presence of an autoimmune disease has been linked to a fivefold increase in the risk of epilepsy. In one series reported by Bien and colleagues (see Bibliography below), one-fourth of patients with adult-onset temporal lobe epilepsy and hippocampal sclerosis were considered to have an autoimmune etiology for their disease. In another study of 114 children with new-onset epilepsy, Suleiman et al. (see Bibliography) found that 9.7 percent were positive for one or more neuronal autoantibodies.
Despite such findings, the precise role of these antibodies in many cases is still unclear. At the same time, the absence of known antibodies does not exclude an autoimmune etiology, and clinicians must rely on other markers, as illustrated in this case. At present, well-characterized case studies remain the best way to understand the role of autoimmunity in epilepsy.
Advertisement
Dr. Moosa Naduvil, aka Ahsan NV Moosa, is a pediatric epileptologist in Cleveland Clinic’s Epilepsy Center.
Dr. Zeft is a pediatric rheumatologist with Cleveland Clinic Children’s who specializes in autoimmune disorders.
Bien CG, Urbach H, Schramm J, et al. Limbic encephalitis as a precipitating event in adult-onset temporal lobe epilepsy. Neurology. 2007;69:1236-1244.
Dalmau J, Gleichman A, Hughes E, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008;7:1091-1098.
Moosa ANV. Autoimmune epilepsies. In: Wyllie E, ed. Wyllie’s Treatment of Epilepsy: Principles & Practice, 6th ed. Philadelphia: Wolters Kluwer;2015:419-425.
Ong MS, Kohane I, Cai T, et al. Population-level evidence for an autoimmune etiology of epilepsy. JAMA Neurol. 2014;71:569-574.
Suleiman J, Wright S, Gill D, et al. Autoantibodies to neuronal antigens in children with new-onset seizures classified according to the revised ILAE organization of seizures and epilepsies. Epilepsia. 2013;54:2091-2100.
Advertisement
Advertisement

New study advances understanding of patient-defined goals

Testing options and therapies are expanding for this poorly understood sleep disorder

Real-world claims data and tissue culture studies set the stage for randomized clinical testing

Digital subtraction angiography remains central to assessment of ‘benign’ PMSAH

Cleveland Clinic neuromuscular specialist shares insights on AI in his field and beyond

Findings challenge dogma that microglia are exclusively destructive regardless of location in brain

Neurology is especially well positioned for opportunities to enhance clinical care and medical training

New review distills insights from studies over the past decade