Response team expedites real-time multidisciplinary interventions
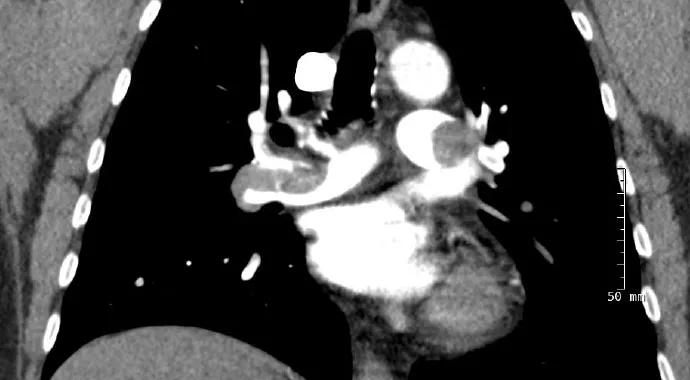
Of the 300,000 to 600,000 cases of pulmonary embolism (PE) in the U.S. each year, 10 to 30 percent result in death within one month of diagnosis, according to data from the Centers for Disease Control and Prevention. In cases of severe PE — i.e., involving abnormal vital signs, right ventricular strain, central or saddle PE, or a large embolism and contraindications to anticoagulation — complex decision-making is often required in a narrow time window if death is to be averted.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In response to these stark realities, Cleveland Clinic has taken an “all hands on deck” approach in the form of a new multidisciplinary Pulmonary Embolism Response Team (PERT) to streamline the care of patients with severe PE.
“The goal is to enable coordinated, real-time consultation by a multidisciplinary team that is empowered to rapidly make complex therapeutic decisions and mobilize the necessary resources for management,” explains John R. Bartholomew, MD, Section Head of Vascular Medicine in the Department of Cardiovascular Medicine and a leading PERT member.
The PERT’s hallmark is its multidisciplinary makeup, consisting of specialists in vascular medicine, cardiothoracic surgery, cardiology, interventional radiology, pulmonary and critical care medicine, emergency medicine, and internal medicine. “The idea is to virtually bring together this diverse team of experts for these complex cases rather than having just one expert making all the decisions in the field,” says pulmonary and critical care specialist Gustavo Heresi-Davila, MD, another PERT member.
As soon as a case of severe PE is identified, the team is activated via a dedicated pager number (2-PERT) for an online meeting (via email or instant messaging platform) followed by a bedside meeting with PERT members joining in person (if needed) or virtually. The team jointly devises recommended management — drawing on resources in the OR, catheterization or interventional radiology labs, electrophysiology lab, vascular ultrasonography suite and beyond — for targeted implementation within 180 minutes (or less) of patient presentation.
Advertisement
PERT implementation began in summer 2014 and was fully completed by January 2015. More than 20 cases had been managed by the PERT by the end of last year.
Advertisement
Advertisement

A sampling of outcome and volume data from our Heart & Vascular Institute

Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery

Large retrospective study supports its addition to BAV repair toolbox at expert centers

Young age, solid tumor, high uptake on PET and KRAS mutation signal risk, suggest need for lobectomy

Surprise findings argue for caution about testosterone use in men at risk for fracture

Residual AR related to severe preoperative AR increases risk of progression, need for reoperation

Findings support emphasis on markers of frailty related to, but not dependent on, age

Provides option for patients previously deemed anatomically unsuitable