A panel of experts studied 26 equations and recommends the eGFR 2021 CKD-EPI creatinine equation

In the United States, more than 37 million adults are estimated to have chronic kidney diseases and approximately 90% of those aren’t aware they have diminished kidney function, according to the National Kidney Foundation (NKF). A consistent method for diagnosing kidney diseases is imperative, however the existing equation that’s widely used to measure the estimated glomerular filtration rate (eGFR), which assesses the body’s ability to filter toxins or waste from blood, includes a race variable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In September 2021, the NKF and American Society of Nephrology (ASN) Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Diseases released its final report outlining a new race-free approach to diagnose kidney disease. The task force recommends adopting the eGFR 2021 Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine equation.
“We recognize what a genetic mosaic we all are,” says Crystal Gadegbeku, MD, Cleveland Clinic’s Chair of Kidney Medicine and a member of the task force. “Not only is race a poor proxy for genetics, but it’s a social construct. So, taking race out of the eGFR equation makes sense.”
The task force engaged with nearly 100 experts from seven countries in weekly meetings for a year.
“As a group, we unanimously agreed that race should not be considered as a factor in estimating GFR,” says Dr. Gadegbeku. “Then we looked at all the potential equations that we could possibly use. We also took into consideration that the equation must be widely-available and easily-implementable. If the most precise equation is not accessible throughout the U.S., then what good is it? With an estimate of over 200 million measurements performed annually, we need a tool that can be used every day in every clinical practice setting, not only to manage kidney disease but for assessment across the spectrum of kidney function.”
The task force examined 26 equations, considering assay availability, standardization, performance and medical consequences. It examined populations used to derive equations, past clinical studies and reviewed new science.
Advertisement
The CKD-EPI is a creatinine-based equation that excludes race, but includes age and sex. Two other previously-derived equations, the CKD-EPI cystatin C equation and the CKD-EPI cystatin-creatinine equation, were compared to the new CKD-EPI equation in a recently published study in the New England Journal of Medicine. The study shows that the CKD-EPI equation is more accurate and led to smaller differences between Black and non-Black participants than new equations without race with either creatinine or cystatin C alone.
The new eGFR equation isn’t the sole recommendation of the task force. “This represents an advancement, but it’s still a tool just like any tool in medicine,” says Dr. Gadegbeku.
The CKD-EPI creatinine equation can be used to estimate kidney function, but primary care physicians shouldn’t base critical medical decisions on a single number. Instead, the estimates should help guide treatment decisions. Dr. Gadegbeku advocates for reporting a GFR range so that physicians and patients understand that these are not precise measurements.
In some cases, additional confirmatory testing or nephrology referral may be necessary. For clinical decisions where greater accuracy is important, the task force recommends using cystatin C combined with serum creatinine to confirm kidney function.
In addition, Dr. Gadegbeku advocates for more research to better understand how the new tool performs. “We need to validate the new approach to eGFR in all types of people, in all ethnic groups, to ensure it is the best approach for a race-less eGFR measurement.”
Advertisement
Perhaps equally important to the creation of this new GFR tool are the larger implications.
“The Task Force is proud to have developed a comprehensive data-driven approach to examining algorithms including race that serves as a model for all other race algorithms in medicine,” says Dr. Gadegbeku. A 2020 article in the New England Journal of Medicine examined race adjustments in 13 clinical algorithms across specialties, from cardiology to pulmonology – and the list was not exhaustive. However, Dr. Gadegbeku warns against simplifying the issue of race inequality.
“The disparities we see in kidney heath were there before the tool was created and will be there even if we develop the perfect tool,” she says. “We have so much to do beyond this tool – even beyond healthcare – to address disparities. There are issues around access to care, insurance, socioeconomic factors and much more. The tool is not a panacea.” But it is a step in the right direction.
Advertisement
Advertisement

Clinicians should individualize dosing practices based on patient risk factors and preferences
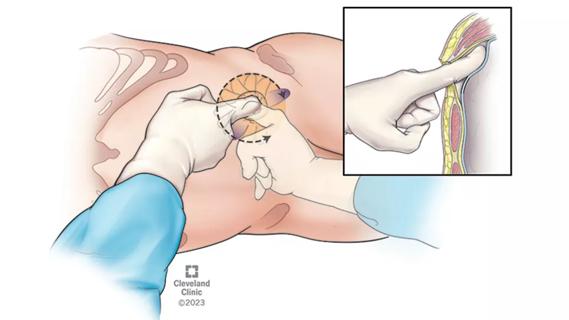
Pioneering and refining the approach in pyeloplasty, nephrectomy and more

Fully-automated process uses preop CT, baseline GFR to estimate post-nephrectomy renal function

Could mean earlier treatment, but also could have negative effects

Unlike earlier pills, new drugs do not cause liver toxicity

Male factors play a role in about half of all infertility cases, yet men often are not evaluated
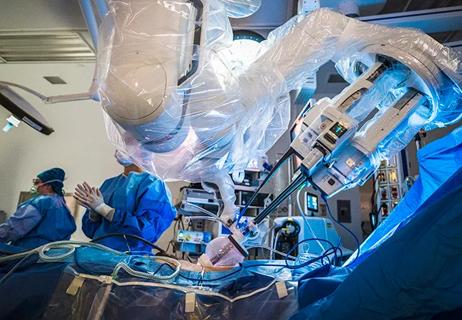
Surgeons choreograph nearly simultaneous procedures, sharing one robot between two patients

Identifying barriers in the renal genetic assessment of Black patients